Introduction
Obese children have different rates of comorbidity with other physical disorders, including chronic diseases such as high blood pressure, diabetes, and musculoskeletal disorders (especially osteoarthritis) when compared to normal-weight children.1,2,3,4,5,6,7 These comorbidities occur similarly across all ethnic groups; however, Mexican-American children seem to have a higher risk of obesity than other groups.8,9 Although the determinants of childhood obesity for children of Mexican descent are likely to be different depending on whether they reside in Mexico or in the United States (US), the prevalence is similar regardless of the country of residence (US or Mexico). The prevalence of obesity (2009–2010) among Mexican-American children aged 6-11 years living in the US was 39.0% (overweight) and 22.1% (obese). Among adolescents 12-19 years, 30.0% were overweight and 16.1% were obese.10 The Mexico National Survey of Health and Nutrition 2011-201211 reported that among children 5 to 11 years old, 19.8% were overweight and 14.6% were obese. For adolescents aged 12-18 years, according to ENSAUT 2012, 21.6% were overweight and 13.3% were obese.
Similar comorbid conditions tend to cluster within ethnic or racial groups, suggesting the possibility that environmental factors may play a role.12 Even though Mexican children living in the two different countries (US or Mexico) confront different economic, social, and safety conditions, poor children in either country might be exposed to very similar patterns of disparities and disadvantages. Some authors have explained this phenomenon by stratifying ethnic and racial groups into further sub-groups (intra-racial groups) whose members range from those who are affluent (higher socioeconomic status) to those who confront numerous disparities.13,14 The focal point of interest in these findings is that intra-racial differences provide a better perspective of the physical and mental health of groups rather than simply a consideration by ethnicity or race alone. In fact, these considerations can explain why previous studies of the same racial or ethnic groups have produced different results (e.g., an association or its absence), as well as apparent discrepancies. For example, there have been conflicting results from research exploring the relationship between obesity and mental health within a sample population (e.g., within a single racial group), with studies either reporting a relationship15,16,17 or lack thereof.18,19,20,21 For example, studies in Mexican-American children investigating the relationship between obesity and mental health have shown varying results depending on the subgroup analyzed,22 including depression23 or impulse control disorders, only among those with extremely high body mass index (BMI)24 or no negative effects for obese affluent Mexican children.25
We hypothesized that these differences may be caused by the inadvertent inclusion, in some of these studies, of specific intra-racial groups without the proper analysis. Our study investigated the relationship between weight status (i.e., obese, overweight, or normal) and the psychosocial profile of Mexican American children and included only children who belong to a specific intra-racial group (i.e., children living in poverty in the US).
Method
Study design
The study design was cross sectional.
Participants
Information was retrieved from medical records (N = 2237) that were obtained from five university-based clinics in a large metropolitan area on the US-Mexico border from May 2009 to August 2010. Data were extracted for individuals who met the following criteria: aged 6-16 years; of Mexican-American origin; and enrolled in Medicaid, state insurance, or lacking insurance. In addition, they had English or Spanish parents who had provided responses to the P+CBCL, and they had at least three recent clinically measured BMIs in the last nine months. Medicaid, state insurance, or lack of insurance participation was considered an indicator of low socioeconomic status (SES). Exclusion criteria included children with a history of chronic or congenital disease as well as children with highly variable height or weight measurements (e.g., exaggerated increase in weight over short periods). Exclusion of cases was selected because in our experience this discrepancy is mainly caused by measurement or data input error (excluded records represented less than 110 records 5%).
Variables
Potential confounders included age and gender, socioeconomic, and health status. To reduce the effect of confounders, multivariable analysis was utilized stratifying by age and gender. SES and health status were controlled by the inclusion criteria.
Measures
The independent variable of this study (normal weight, overweight or obese) was computed by calculating BMI. BMI was calculated for each child using the formula weight/height.2 We categorized normal weight as children with a BMI ≥ 10 percentile to < 85 percentile), overweight as children with a BMI ≥ 85 percentile to < 95 percentile, and obese as children with a BMI ≥ 95 percentile) using charts stratified by age and gender that are published by the US Centers for Diseases Control (CDC).
P+CBCL
The P+CBCL is a pictorial version of the Child Behavior Checklist (CBCL),26 which has been shown to be beneficial among those with communication disparities, such as language, education, and literacy.27 The P+CBCL is an exact version of the original written CBCL but include visuals (pictograms) to help parents better understand and respond to the questions. It includes 120 behavioral and emotional problem items that assess a child’s behavior on a 3-level scale for rating the extent to which a parent perceives each item in their child (0 = not true, 1 = somewhat or sometimes true, 2 = very true or often true). According to the authors of the CBCL, factor analysis of the CBCL items yields eight syndromes: three syndromes (Withdrawn, Somatic Complaints, Anxious/Depressed) load on the broadband internalizing factor, two (Rule-Breaking and Aggressive) load on the broadband Externalizing factor, and the other three (Social Problems, Thought Problems, and Attention Problems) do not load differentially on either broadband factor. A Total Problems score is computed by summing all problem items. This assessment has reported a high test-retest reliability (e.g., mean r = 0.90 SD = 0.03 for empirically based scales) and strong internal consistency (e.g., Cronbach alpha = 0.97 for Total Problems score). Higher scores on these scales are associated with more psychosocial and behavioral problems. Raw scores are converted to T scores to determine scores in the normal and clinical range. T scores of 65 and higher are considered the clinical/subclinical cutoff points for the syndrome scales; 60 and higher for total and problems subscales.
Statistical analysis
Categorical data analysis was reported using means and standard deviations.
Statistical differences on multiple continuous dependent variables (MANCOVA) by an independent grouping variable, while controlling for a third variable called the covariate, are suggested for this type of analysis in other studies using similar data.28,29,30
Multivariate ANCOVAs (MANCOVAs), all of which had a 3 (weight category) × 2 (gender) × 3 (age groups 6-9, 10-13, 14-16) design were run for internalizing and externalizing problems and the eight empirically based syndromes. Alpha was set at p < .01 to take into account the multiple analyses.
Effect sizes, measured by partial Eta squared (ES), were characterized using Cohen’s31 criteria (small = .01 to .06, medium = .06 to .14, large > .14).
Statistical analysis was conducted using Statistical Package for the Social Sciences (SPSS) V20.0.
The study received institutional review board approval.
Results
This study included 2237 patients, with 1108 (49.5%) girls and 1129 (50.5%) boys. A total of 1292 (57.8%) participants had normal weight, 353 (15.8%) were overweight, and 592 (26.5%) were obese. The mean age was 9.92 years (SD = 3.01).
Effects of weight category, gender, and age in the P+CBCL transformed raw scores
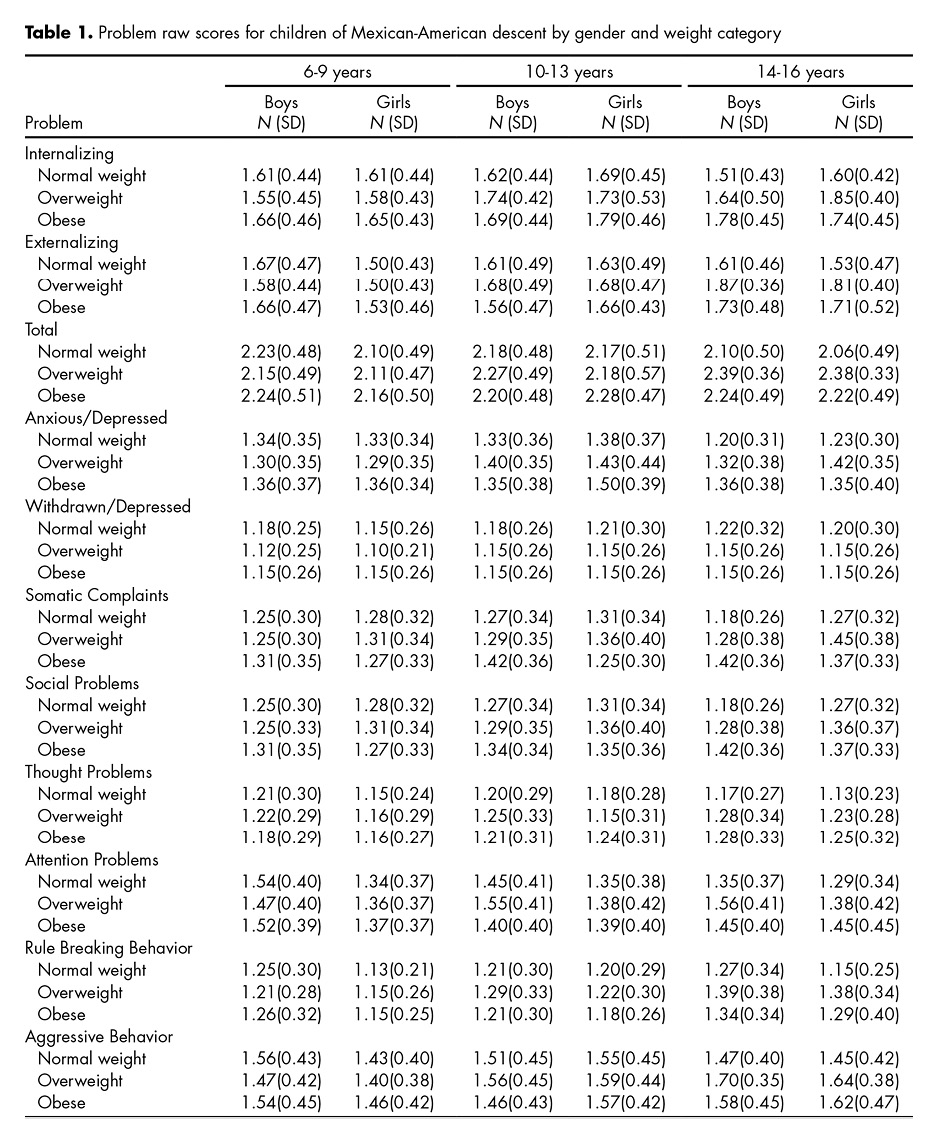
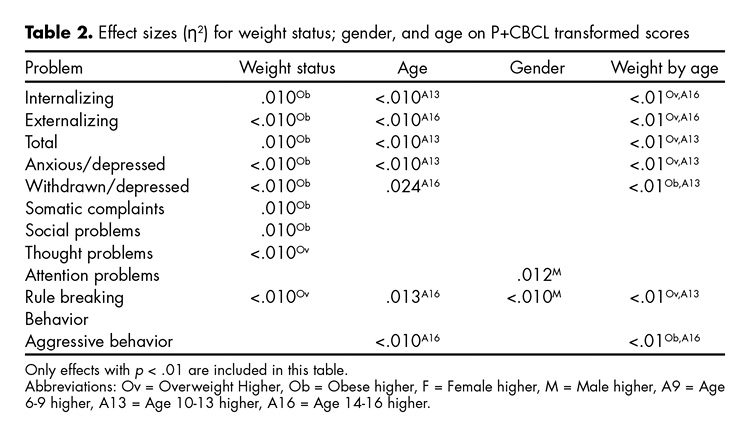
The eight P+CBCL subscales were not normally distributed; therefore, a transformation was performed with a logarithmic transformation that included adding the value of one to each subscale because some individuals had values of zero, precluding logarithmic transformation. The transformed raw scores for the main syndromes are displayed in table 1 by weight category, age group, and gender. In table 2, partial effect sizes (ES) values for all significant effects (p < .01) are displayed in the MANCOVA on P+CBCL transformed scores. As shown in table 2, main effects for weight categories were found for six problem scales as well as Internalizing, Externalizing and Total problems (all ESs ≤ .02). In all scales, obese children had the highest scores, with the exception of Thought and Rule-Breaking problem scales. For these categories, overweight children obtained the highest scores.
Significant age effects were found for seven scales (all ES < .03). Children aged 10-13 years had higher scores than younger or older groups for Internalizing, Total, and Anxious/Depressed Problems. Adolescents 14-16 years old had higher scores for Externalizing, Withdrawn Depressed, Rule Breaking, and Aggressive Behavior problems.
Significant gender effects were found in two scales. Males scored higher than girls in Attention and Rule Breaking problems. The only significant interaction involved weight status by age group (all seven scales ES < .01). Internalizing and Externalizing problem scores were higher in overweight children in the 13-16 years old age group. Total, Anxious/Depressed, and Rule Breaking problems scores were highest in the overweight children aged 10-13 years old. Withdraw/Depressed problem scale scores were highest among obese children in the 10-13 years old age group, and Aggressive problem scores were the highest in obese children aged 13-16 years old.
Discussion and conclusion
The results of our study suggest that obese and overweight children living in poverty reported a higher risk for mental health problems when compared with normal-weight children living in poverty. The psychosocial profile of this intra-racial group by weight category indicates higher scores in both internalizing and externalizing problems for obese boys and girls. While problems were more frequent among children in the 10-13 and 14-16 age groups, the interaction of the variables of weight category and age grouped suggest more problems in the overweight group of 10-13 years old.
Overweight or obesity among children living in poverty had an effect on their emotional and behavioral problems. Poverty by itself places children at risk of emotional and behavioral problems. In addition, poverty has an effect on obesity prevalence, with higher levels of obesity linked to lower socio-economic status.32 While race and ethnicity may affect the relationship between socio-economic status and obesity, consideration of intra-racial differences and accounting of disparities can better explain the results.
Disparities tend to have a stacking effect; usually, poverty is not the only disadvantage that a child confronts. Violence, lack of a healthy lifestyle or cognitive stimulation, parental unemployment, and/or lack of social opportunities surround the lives of these children. Our assumption about the low effect size reported in this study is that the psychosocial profile obtained in this sample might not be completely explained by their weight status and poverty levels. Instead, it is possible that obesity is one of many other factors that contribute to the mental health of children along with the possible additive effect of other disparities.33 Yet, there are important implications for the health care of children when considering both intra-racial group differences among ethnic groups, as well as the hidden combined effects that the exposure to disparities can have on a child.
Strategies to prevent childhood obesity in the primary care level and future consequences have not yet succeeded. This failure suggests the need to explore different types of healthcare delivery for those confronted by disadvantages. The current healthcare system is not currently providing the additional support needed by families that confront disparities encountered mostly among minority groups or those living in poverty.34 This additional support is needed to help families confronting disparities reduce the continuous and systematic exposure to health risks.35
There are limitations in this cross-sectional study that include the causal relationship between obesity and psychosocial and behavioral problems: Did overweight and obesity lead to psychosocial problems, or did psychosocial problems lead to inactivity and/or overeating, which then lead to obesity? In addition, due to the restriction on only selecting children with three clinical measurements, there is a possibility that the prevalence of overweight and obesity in this population of Mexican-American children living on the border was higher than we report. Because this was not a comparison with children of higher SES, we cannot assume that the results found are not similar in all Mexican-American children. Previous research has well established the consequences of obesity for physical health; however, the impact of obesity on psychological well-being is less clear.17 Despite the limitations of this study, we found that obese and overweight children living in poverty reported a higher risk for mental health problems than did normal-weight children living in poverty.
Regular care offered to these children from intra-racial groups need an additional investment including a systematic support for their families, perhaps through parent education, that will remediate the effects of environmental risk exposures (violence, addictions, etc.) and encourage changes to their unhealthy lifestyles (obesogenic, sedentary, addictions, etc.).36 In addition, it is necessary to provide families with simultaneous management of their comorbid conditions in order to effectively prevent and treat these problems. Addressing only one problem (e.g. obesity) might not result in the best outcome due to the co-existence of other problems (e.g. mental health).
This study suggested that Mexican-American children living in poverty may represent an intra-racial group. Morbidities and co-morbidities confronted by these intra-racial groups of children are common not only among Mexican or Mexican-American children, but also among all children living under these conditions. Research studies must consider children’s race-class groups instead of only classifying them by their racial group to improve the accuracy of their findings. The range of cultural and family characteristics can only partially explain differences between racial or ethnic groups; however, these differences could be better explained by taking into consideration the diverse profiles among individual race/ethnic groups.37,38
Future studies should focus on strategies for further understanding the possible implications in research and clinical care of intra-racial differences among Mexican-American children confronted by disparities.
Funding
This study was funded by the Department of Pediatrics – Texas Tech University Health Sciences Center.
Conflict of interests
All authors have no conflict of interest to declare.