Introduction
Obesity is a growing problem in children and adults. Its implicit consequences and risks have been widely documented. Mexico´s case is alarming (Gutiérrez et al., 2012). Despite the overwhelming evidence from numerous publications, we are still lacking an effective and viable public health solution (Boon & Clydesdale, 2005; Garner & Wooley, 1991; Müller & Danielzik, 2007; Thomas, 2006).
At the core of the obesity problem we find the energy imbalance in the human body whose physical activity falls short of using up the ingested energy (Müller & Danielzik, 2007). This view of the problem is essential but it is also insufficient for planning and implementing interventions against obesity, be them preventive or reductive (Maziak, Ward & Stockton, 2008).
Many interventions (Boon & Clydesdale, 2005; Garner & Wooley, 1991; Kelly & Melnyk, 2008; Khambalia, Dickinson, Hardy, Gill & Baur, 2012) − from physician’s prescriptions all the way down to nationwide campaigns, programmes and public health plans − basically entail threatening people with the negative consequences of obesity, informing them about foods they should avoid or eat and stating the importance of physical exercise.
Although we know that we cannot prevent obesity without achieving an energy balance, we also know that such a balance depends on a vast and complex network of psychosocial, cultural, and behavioural elements (Bray & Champagne, 2005; Karasu, 2014; Rosenkranz & Dzewaltowski, 2008). The literature documents the influence of the physical (Addy et al., 2004; Ball, Timperio & Crawford, 2006), family (Elder et al., 2010; González-Rico, Vásquez-Garibay, Cabrera-Pivaral, González-Pérez & Troyo-Sanromán, 2011), and school environment, both in high-density food consumption and in the promotion of sedentary habits. The availability of these foods and the absence or deterioration of places to exercise; time distribution and family tasks; and parents and teachers as negative behaviour models for the children, all contribute to increase obesity. Nevertheless, we do not know the complex network of these influences, nor the interaction and feed-back loops between them (Hammond, 2009). Although interventions and programmes against obesity include psychological, social, and cultural elements, the range of problems and the resources of any given family can be so specific that general solutions are rendered useless in practice (Khambalia, et al., 2012).
Our objective was to broaden our understanding of the child obesity problem from a bio-medical perspective all the way to a community mental health approach, able to ground more comprehensive and sustainable interventions. For our research question we sought to ascertain how the influence of the environment and the behaviour of the family interact to construct obesity in children. We trust that this information will help us rethink the nature, content, and instrumentality of health interventions in order to prevent and fight obesity (Elder et al., 2010). We also want to include in our understanding of the problem its prevention and treatment; the daily life of the community, school, and family, the resources of the latter and its interaction with the surrounding environment (Russell-Mayhew, McVey, Bardick & Ireland, 2012).
For this purpose, we designed the present qualitative study that interprets the results of interviews and observations with a sample of social actors involved in the community construction of obesity. In this study, we deal with school children from one of the marginalized areas of Mexico City where health conditions are even more precarious and the psychosocial elements are more complex than in the rest of the city (Garner & Wooley, 1991).
Method
Type of study
To fulfil the objective of broadening our outlook on the obesity problem and of building a new theory based on the data provided by the social actors, we carried out a field study using the Grounded Theory method. This method was also selected in order to include in the model the different groups of social actors, their interactions and contexts, as well as the social structures in which the problem is immersed.
Characteristics of the research team
The Principal Investigator of this project is a full-time researcher at the Instituto Mexicano del Seguro Social (Mexican Social Security Institute [IMSS]), dietitian and Doctoral Candidate in Health Sciences. The research team was made up by one PhD in Social Psychology who is a university professor, and two RDs with Masters and BS degrees in Nutrition Sciences, one a full-time researcher and the other one a student hired for the project. Six BS Nutrition Science students, trained by the researchers, carried out most of the interviews under their supervision and also helped with data coding. All team members have experience in child nutrition projects as well as in community interventions.
Setting
The present study was carried out in three elementary schools of a marginalized area of Mexico City. This is the suburban area west of the city where the streets layout is erratic and visibly improvised around the uneven landscape. Urban services such as sewage, water, electricity, etc., fail frequently. Most homes were self-built with cheap materials. Population density is high and the school facilities are in a bad shape.
Conditions are similar in all the schools in the area and those that took part in the study were included because of the willingness of their authorities to participate.
All nine classrooms we used were equipped for school activities with acceptable lighting and worn down furniture, but good enough for an interview.
Participants
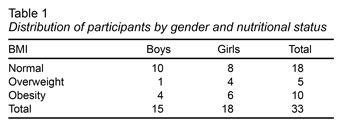
In order to cover the possible variations in the concept of obesity and its construction, we utilised theoretical sampling (Corbin & Strauss, 2014). This means that we included in the study all those types of social actors that could have different views on the problem of obesity. Boys and girls with obesity or overweight and others with a normal Body Mass Index (BMI) (Table 1) were included in the study. They were measured and weighed for a total of 33 boys and girls. None of the children refused to participate, and therefore none were excluded.
The analyses of the first interviews showed the importance of parents and other adults in the children’s nutrition process and put forward the need to include other social actors in the sample (Richards & Morse, 2013). Some of the children’s mothers accepted our face-to-face invitation to come to the school for an interview. The children were informed about the interview with their mothers, but the latter were not present to avoid mutual influence. The only condition that excluded mothers from taking part was lack of time. None of them showed any resistance or suspiciousness towards the project.
Instruments for data collection
The semi-structured interview guide included questions about the nutrition process in the family, the school, the street, the children’s physical activity, their exposure to advertising and junk food availability, any help they could have received against obesity and their own behaviour on the subject. Each interviewer made sure that the guide topics were covered with the intensity that the interviewee chose. New open questions served to probe into incomplete themes.
All co-authors recorded in field journals their non-participant observations at the schools and the community at large.
Procedure
After a familiarization process with the schools and introducing the researchers to the participants and explaining the purpose of the study, the second and fourth co-authors, along with a team of students, carried out in-depth interviews with the three types of social actors.
After being introduced to the children, a researcher interviewed each boy or girl. The child’s teacher could sit in, quietly, in a different area of the classroom, with no other children present. We ushered each child discretely to his or her interview, avoiding exposing them in public as participants. We never mentioned their diagnostic or their BMI. Interviews and observations lasted about half an hour with each participant ‒ teachers, mothers or children ‒, and they were carried out throughout a period of three months, between February and May of 2012. All interviews were finished in a single session.
Analysis
All materials were transcribed and analysed as free text using NVivo9 (QSR International, 2012). The researchers transcribed and coded the interviews themselves. All names were replaced by pseudonyms upon transcribing the audio recordings. The initial categories merely described the nutritional process: food selection and meal planning; grocery shopping, storage, preparation and consumption; food preferences, behaviours and habits of the social actors. The more abstract categories were elicited through analysis and debate among the researchers and by triangulating interviews and field notes. Finally, we searched for relationships of affinity, continuity and opposition, consequence and contingency between categories to elaborate the more abstract theoretical elements of the model. The team would meet frequently to verify and unify coding and interpretation. The analysis delved deeper into the different topics until we found enough repetitions and confirmations for theoretical saturation. As the analysis progressed, the research group developed the concepts and relationships that constitute the Grounded Theory submitted in the Discussion section of this article. In the subsequent phase of the project (that will be reported in future publications upon completion) the interviewed girls and boys were summoned during school hours to look at the preliminary results of the study and to asses their accuracy. Most of the children agreed with the researchers’ findings and when this did not happen, due corrections were made.
Ethical considerations
The research protocol was reviewed and approved by the Ethics Committee of the Centro Médico Nacional Siglo XXI (National Medical Centre XXI Century).
All interviews were carried out in a one-on-one basis in the school classrooms after the class schedule and were audio recorded. Before interviewing the children, the researchers read aloud to the parents a briefing letter, highlighting their right not to participate. Those who agreed signed an informed consent form. In order to avoid adding unnecessary strain to the interviews with children, we only recorded their verbal consent for participation. In order to take care of the individual processes that the interview could initiate, the research team members made themselves available to the children and their parents.
After the data were analysed, the outcomes were reported to the school authorities for verification to contribute to their rigour and to avoid any negative implications for the children and the schools.
The relationship between the interviewers and the participants began with a brief presentation with the children’s groups. In this phase of the study, their face-to-face relationship with mothers and children was limited to the interview in order not to create false expectations and not to skew the information beyond the scope of the study.
Results
A total of 33 children ‒ third and fifth graders between the ages of eight and ten ‒ provided information for the study. They were divided according to their gender and BMI-based nutritional status, as shown in Table 1.
The mean age of the children’s mothers was 37.8 years and ranged between 18 and 70 years. Of all parents in the study, 6.3% of them had a college education; 10.9% finished high school; 20.6% finished junior high school, and 20.6% finished elementary school. The rest reported no studies at all; 46.1% were formally employed; 12.6% were informal traders, and the rest had informal jobs other than retail.
Within these participant’s responses, we found the themes that show, on one side, the strong forces that push unhealthy foods and behaviours into their lives and, on the other side, the weak resources that do not suffice to keep their health. We will explain how these two groups of forces are combined in what we call Psychosocial Imbalance.
Toxic environment
In this section we will show how obese children as well as their classmates are surrounded by an environment that favours energy imbalance in spite of their poverty. This environment consists of a high availability and persistent publicity of high-density foods, the lack of effective regulations, the influence of peers, and the promotion of a sedentary life.
Availability and promotion
Industry produces high-density foods and uses a variety of means to make them physically and economically available and appealing to the children. One boy, in dialogue with the interviewer, said:
I: Do they [your parents] ever, as a reward, take you out to eat?
N: Yeah.
I: Where?
N: Tacos and McDonald’s or to KFC.
I: All right, tell me. How is that?
N: It is big. There is a playground and soft drinks. If you want more soft drink you go and order and they don’t charge you. (id 2022, obesity, age 10)
Lack of regulations
Government regulations that could buffer the influence of the food industry are minimal and are neither part of a coordinated program, nor evaluated for modifications. In any case, our participants perceive that the government has choosen to do nothing about the children’s obesity. One teacher told the interviewer:
I: And, what do you think about the children drinking so many soft drinks? […] Who do you think is responsible?
T: there are many culprits: The government that puts no limit on the companies. Obviously, as they pay taxes and create jobs and all that… all this is convenient for the government and the economy… but at the cost of the people’s health.
In many cases, the voice of health is limited to a hurried slogan at the end of radio and TV commercials, saying “Eat well”, “eat fruit and vegetables” or something similar that seems to have no impact on children.
Locally, junk food vendors are ever-present outside school premises at start and end times and also at the places where the children hang out. One girl, at school, told one of our interviewers:
I: Hey, and, what do they sell here in the morning before school starts?
N: They sell corndogs, jicamas, ah… yoghurt, “gorditas”, Cheetos, two-peso freezies, caps and t-shirts.
I: I mean, food.
N: Food? Several candies; and also “tlacoyos” (filled corn pancakes). (id2060, normal, age: 9)
Peer influence
Besides pressure from advertising campaigns and indulgent adult family members, children are exposed to peer influence to eat high-density foods any time of day. A boy told the interviewer:
I: And if one day your friends, you best friends from school are playing together at recess and are eating something new that you have not tried and you join them, what do you do?
B: I buy myself one.
I: You buy one to try it? Why?
B: To find out what it tastes like.
I: Sure. Would you be curious because your friends had one?
B: Yeah. (id4042, obesity, age: 10)
Sedentarism
This toxic environment is not limited to the presence and promotion of unhealthy foods, the chances of these children for physical activity are also under attack by the industry and advertising. Once again, the community’s socio-economic conditions would suggest more walking and less use of technology. But this is not the case. These children’s families can afford video games and other sedentary activities that have replaced sports and open-air games. One overweight child said:
I: When you play on your computer, how long do you do it for?
N: Half an hour.
I: Half an hour. And, how about video games?
N: Video games like…
I: Nintendo, Wii, Play-station.
N: Yeah, Play-station.
I: Do you have it at home?
N: Yes.
I: And, how long do you play for?
N: I don’t know, I don’t remember, because I always play all day long. (id2055, overweight, age: 9)
Children spend more and more time sitting in front of a screen. Backed by availability and advertising campaigns almost as effective as those for junk food, sedentary activities take up most of the children’s free time.
Upon talking with people we realised that the opportunities to practice organised sports are very scarce in these neighbourhoods. Outside the schools and around the community the spaces for physical activities are, on the one hand, scarce and, on the other, unsafe due to the presence of gangs or drug users. The parents, would rather have their children stay at home. One girl said:
I: Hey, K., close to your house, is there any park or sports place you can go to?
K: Yes, but it’s very ugly.
I: Why is that?
K: Because there are many bums and all that. Besides, we are not allowed to go there alone.
I: Who do you go with?
K: With my granny, I have to go with her, or with my Mum.
I: And, do you go there often?
K: No. (id2053, overweight, age: 9)
In brief, we can see that the children are surrounded by a variety of forces; some social like peer influence or dangerous parks, and some psychological, like publicity, that push high-density foods and inhibit physical activity. This interplay constructs the energy imbalance.
Ideally, a child and his family could take some actions to face these forces and maintain a healthy weight. In reality, we found that these families have only scarce resources to resist the toxic environment (Garner & Wooley, 1991). We will describe this scarcity in the following section.
Shortage of family resources
Immersed in this toxic environment, the overweight child’s family could decide what the child should eat at home and school and also make sure he/she exercises. In our sample, the family resources were reduced by misinformation, food indulgence, other family demands, social vacancies, and insufficient actions. Our findings show how these combine to turn the odds against health.
Information and knowledge
The first resource is nutritional information. Among our participants, it is scarce and, in many cases, wrong. About the problem per se, some parents do not know that their child is obese or overweight. Other parents know it, but they do nothing about it. They accept that the child is “a bit chubby”, but not much more. They have incorrect notions about the aetiology of obesity, about the weight and height that define it, and about the way to control it. The mother of an obese child said:
I: Then… what do you think is the cause of the problem that G. has this excessive weight?
M: Well, honestly, at the moment I do not see it as a problem.
I: Why?
M: No… I do not see my child having a problem that is very… Maybe he does, but very slight and, as I said, I have searched for a solution and the doctor tells me: but, no, I find him very healthy. (id1021, obesity, age: 10)
Most of these children’s parents are not interested in the nutritional information about the food that they provide nor do they know what type or amount of physical activity is enough to maintain one’s health. Many of them tell us that they should eat less fat and carbohydrates and that they should eat more fruits and vegetables. They also know that the children need exercise but none of these pieces of information that the parents can express generates ever any concrete or effective action. They modify neither their own diet nor that of the children and the same goes for their physical activity patterns.
Food indulgence
At home, the children’s diet often includes processed foods, or traditional fried dishes with a high fat and sugar content, that the children like and the adults in the family find convenient because the children accept them readily and they are easy to prepare. The food industry makes them readily available and at a relatively cheap price. Abundant and effective advertising creates the need for consumption that parents permit. A girl told us:
I: …something new, what cereal do you buy?
N: Cereal?
I: Yeah.
N: Corn Pops.
I: Sure and, those, how did you find out about them?
N: On TV.
I: Yes and, who did you ask to buy them for you or why; how did you get to try them?
N: I asked my Dad to buy me some Corn Pops. He got them for me and they taste good.
I: You did like them and, do you only ask for those or do you sometimes get another kind?
N: I only ask for those. (id1088, normal, age: 8)
Family allocation of resources
Even those few families that have adequate information about the nutritional status of their children and the way to care for them have problems implementing it. The family’s resources are scarce and are allocated to the satisfaction of needs that the family considers as priorities over the children’s weight control. These resources are not only time and money. Our fieldwork revealed that health maintenance also demands the parents’ attention, the children’s attention and compliance with the parent’s directions, and the self-control of both, parents and children, since the parent’s nutritional behaviour and the example they set is not healthy either. Even if it is not evident at first sight, these resources have to be administered and are limited. The parents prefer to save their family’s social resources and their own influence on their children for the children’s homework, for instance, or for keeping them away from drugs. In a typical family moment, once the children have done their homework, the parents gratify them with food choices and use of their free time. One girl explained:
I: Is there anything you are not allowed to eat?
A: Hm. Cheetos.
I: Why?
A: Because my mum says they are not good for you.
I: And, has she told you why they are not good for you?
A: No.
I: Just like that? And, do you eat them or not?
A: Sometimes she lets me have some and then not.
I: When does she let you have them?
A: Like ah, she lets me eat them when… sometimes when I help her she tells me: grab something, if you want, have some Cheetos; and then I get them and that’s it.
I: Where do you grab them from?
A: From the store. (id2031, overweight, age: 9)
Social vacancies
Finally, we found that within the families there are some nutritional functions, such as food selection, storage, and preparation, which are not formally assumed by any member of the family. Most meal times are not planned; they are improvised around indulgence and ease of preparation. In many cases, this is done by a social actor who is not a member of the family. In the field journal of one of our researchers, we read:
“The grandmother is in charge of the girls’ meals three times a day. However, she is unaware of the rest of their nutrition process. It seems that none of the caretakers really knows what the girls ate because each one has incomplete information.” (FJ3)
The same applies to supervising and attending physical activities. The parents don’t have the time or prefer resting to sharing these activities with their children. Most of the children do not play outdoors because they don’t like to be on their own. These social vacancies lead to a series of improvised and disconnected nutritional events that privilege comfort, indulgence or the taste of foods over health.
Insufficient actions
The adult family members make short-lived and isolated attempts to revert their children’s obesity. These efforts are not constant or coordinated enough and are based on misconceptions and sporadic information from the media or from health professionals. There is a lack of formal commitment to any given strategy. The mother of an obese child told us:
“[…] for example I, maybe these are just excuses or lack of responsibility, or not, I do not know what it is, but, well I’m going to do it, but I don’t or maybe I do it only once. For example the time we attended a lecture on nutrition, the first few days after the lecture, we were all keen on giving the children fruit, and so… but later, we all forgot about it, all of us.” (id 2083, obesity, age: 9)
In these endeavours, the absence of professional assistance and public health organisations is significant. Actions for treatment or prevention are only partially implemented or only for a short time, under the caveat of not disturbing the children or taxing their obedience. Many of these interventions are limited to “diets” that the children soon abandon. The field journal of one researcher reads:
“The interviewed sixth grade girl, according to her grandmother, was subjected to a diet provided by health professionals, but ‛she could not stick with it’ and then she quit and replaced it with a ‛natural’ diet. They give her smaller helpings of certain foods, but her sugar intake is still quite high.” (FJ2)
Summary
The families in our sample, especially the children, live surrounded by high-density foods, which are readily available and advertised by the media. They also live in an urban and social environment that discourages physical activity. The conditions, habits, and resources of these families do not allow them to resist the obesogenic environment. The available professional assistance issues plans and strategies that are too broad, too demanding, unrealistic or restricted to lists of foods and warnings about the consequences of obesity. The forces that promote these undesirable foods are far greater that those any family could ever muster to preserve the health of its members. This is what we call Psycho Social imbalance.
Discussion and conclusion
The present study was carried out in only one school area and with schools that were willing to participate. We also selected those participants that could better shed light on the problem. Consequently, and given its initial exploratory and explanatory intent, we did not set out to demonstrate relationships between variables, but rather to embark upon a path of in-depth understanding of the problem. We trust that our findings are a starting point to approach child obesity and avoid previously ignored obstacles.
The concept of energy imbalance is present as a basic biological element of obesity, but its descriptive capability is very limited (Russell-Mayhew et al., 2012). It could be said that, combining nutrition and physical activity in that equation, incorporates behaviour and social environment in a more interdisciplinary approach to obesity (Kremers et al., 2006). But we are still missing the community health outlook to begin to explain the phenomenon and, thus, inform the intervention.
Our findings show the toxic environment in which high-density foods appear as an opportunistic predator that threatens the children’s health in the different spaces and times of their lives (Gordon-Larsen, Nelson, Page & Popkin, 2006). Obesity is, essentially, a surplus of energy that suggests the presence of a surplus of resources. This community perspective tells us that the industry that produces high-density foods and the media that advertise them have penetrated the marginalized communities in such a way that poverty is no protection against obesity (Wang & Zhang, 2006). On the contrary, poverty contributes to restrict the physical resources, such as time and space, that the family can no longer use to fend off the toxic environment that surrounds their children (Melius, 2013). The same has happened with the sedentary lifestyle. The community’s assumpiton is that eating well and exercising are expensive.
The energy imbalance in overweight children’s bodies is a projection of the abysmal imbalance existing between the power, versatility, and wealth of the junk food industry and the limited resources that the family has and may allocate to health and nutrition. The emphasis that health professionals place on the biochemical imbalance seems to ignore or, at least underestimate, this psychosocial imbalance. Furthermore, its interventions target an ideal family that, in order to control the weight of its members, only requires information and motivation. These intervention models seem to assume that all families have the full array of nutrition and health related family roles necessary to prevent obesity. It is as if families were able to assess their children’s nutritional status (Bray & Champagne, 2005; da Costa, Blanques, dos Santos, 2015; Turnbull, Martínez-Andrade, Huérfano, Ryan & Martínez, 2009) and had someone to plan, supply, store, prepare, and serve food in an organised manner (Karasu, 2014; Kelly & Melnyk, 2008). Such models ignore that the medicalization of obesity (Russell-Mayhew et al., 2012) contributed to create many of these social vacancies.
We found a very persistent, versatile, and almost ubiquitous junk food industry. None of its individual actions is invincible, but they are so many and so varied that families have no way to fight back. This industry thrives on family weaknesses: children’s preferences, the need to please them, parent’s lack of information and time, and many others that take advantage of genetically vulnerable individuals and gradually construct child obesity. Resistance against such an attack would require around the clock attention from parents in order to counteract the influences that increasingly infiltrate daily life as if they were the natural behaviour of people and families. The same happens with the offer of sedentary activities that matches the physical and social limitations of the communities as has been found in other countries (Garner & Wooley, 1991; Gordon-Larsen et al., 2006).
In view of the foregoing, Psychosocial Imbalance can be described as the enormous difference that exists between the power of the toxic environment to promote bad nutrition and the powerlessness of families to cope with it and maintain the nutritional health of their children. Energy imbalance is the outcome of psychosocial imbalance.
Programs and interventions target fictitious families. In these fake families, this imbalance does not exist; children’s nutritional health becomes, in point of fact, a matter of priority and they have all the necessary resources to implement the program (Hoddinott, Craig, Britten & McInnes, 2012).
Any intervention against obesity and overweight should broaden its perspective on the problem, establish realistic goals, and take into account the knowledge of both communities and families upon developing and implementing its goals and activities. Instead of offering average solutions that would only work in average families, programs could be geared to encourage families, through participatory research and action, to evaluate their own situation (Ainslie, 2012), to visualize and capitalize on their assets and face their particular problems with the material and psycho social resources at their disposal (Garner & Wooley, 1991).