Introduction
Relatives of people with borderline personality disorder (BPD) experience a considerable objective and subjective burden. This is the particular case of Informal Primary Caregivers (IPC), who experience half a standard deviation above the mean burden of caregivers of inpatients with other severe mental disorders (Fruzzetti, Santisteban, & Hoffman, 2007). This has been related to the presence of interpersonal problems with the BPD relative due to a lack of knowledge of the disorder, its prognosis, and treatment, as well as limited or non-existent assertiveness skills (Morgan et al., 2010).
The satisfaction of IPCs’ needs –whether for information, training in specific social skills, and/or control of negative emotions– is important per se, and because the evolution and prognosis of relatives with BPD depends largely on the family’s interaction and collaboration (Giffin, 2008). However, although there are interventions with proven effectiveness for family members who care for patients with other severe mental disorders (SMD), such as schizophrenia and bipolar disorder (Del Pino, Palomino, & Frias, 2015), scientific literature has highlighted the absence of effective standardized programs for IPCs of people with BPD (Rapaport, Bellringer, Pinfold, & Huxley, 2006), (McFarlane, Link, Duchay, Marchal, & Crilly, 1995).
This may be due in part to the lack of routine evaluations of these IPCs’ needs (which does not occur in the case of relatives of people with schizophrenia, bipolar disorder, neurological disorders, and terminal diseases) (Tennakoon et al., 2000). In this respect, the objective of the present study was to adapt and evaluate the reliability (internal consistency) of the Questionnaire on Needs of Family Members of People with SMD (QNF-SMD) to detect the needs of the IPCs of patients with BPD, characterize these care needs, and propose evidence-based intervention strategies capable of meeting them in a timely and effective way.
The QNF-SMD was developed in Spain by Gómez et al., (2012) to identify felt and unfelt needs as well as those which have been met or not in caregivers of patients with SMD. It is a self-administered instrument with 27 items grouped into four areas: 1. Knowledge/information: items 1 to 9 refer to the amount of psychoeducational information on the disorder the family member has or needs; 2. Instrumental support: items 10 to 15 concern knowledge of the tools available; 3. Participation: items 16 to 20 are related to the need to participate in decision-making concerning the treatment of their relative; and 4. Personal support: items 21 to 27 explore the need for professional and social support for themselves.
The response options to each item are: “I have felt this need and it has been met”, “I have felt this need, but it has not been met”, and “I have not felt this need.” For comparative purposes, the percentages of needs that have been met, unmet, and not felt are calculated for each area.
The QNF-SMD has been applied to relatives of patients diagnosed with a SMD in two psychosocial rehabilitation centers in Madrid, Spain, showing a satisfactory level of internal consistency. There are more met needs in Knowledge/information (63%), together with an absence of needs in the areas of Personal support and Participation (81% and 84%, respectively), with the highest proportion of felt and unmet needs being observed in Instrumental support (30%) (Gómez et al., 2012).
Method
Adaptation of the instrument
First, an adaptation into Mexican Spanish of the QNF-SMD to assess the specific needs of IPC in patients with BPD (vs. a SMD in general) was undertaken through the evaluation and suggestions of four experts in the clinical care of patients with BPD (three psychologists and one psychiatrist specialized in one form of psychotherapy specifically design for BPD patients [Dialectic Behavioral Therapy, for example] and with at least 10 years of experience treating patients with BPD along 10 or more hours per week).
Reliability and detection of needs
A descriptive, cross-sectional study was conducted on a sample of IPCs of patients with a confirmed diagnosis of BDP attending a public psychiatric clinic in Mexico City, Mexico.
Subjects
A convenience sample was obtained from 80 family members of patients diagnosed with BPD, all literate and over the age of 18, who considered themselves as the IPC, and agreed to participate in the study. According to Nunnally’s (1991) recommendations, the minimal sample size needed to evaluate the internal consistency of each subscale of the instrument was calculated by multiplying the number of items in the area of Knowledge/information, which is the subscale with the most items (nine) by five participants. It can therefore be assumed that the sample size was suitable for psychometric purposes since it included at least 45 participants.
Procedure
The Ethics Review Board of the psychiatric institution where the study was conducted approved the protocol and all the research materials, including the informed consent form. After IPC participants had signed it, the adapted instrument was applied to obtain internal consistency and identify and describe their care needs.
All participants were invited to participate during the psychiatric follow-up consultation and after a psychiatrist confirmed their family member’s diagnosis of BPD through the application of the structured interview SCID-II (First, Spitzer, Gibbon, & Williams, 1995).
BPD patients were asked to attend with the family member who supported them the most in their everyday lives and were told that, if they wished to participate in the study, they only had to answer a self-report questionnaire lasting approximately 20 minutes.
A psychiatrist/psychologist administered the questionnaires at the clinic. When patients finished the questionnaire, the psychiatrist/psychologist who administered it checked if all questions were completed and, when necessary, asked patients to do so in order to avoid missing data. Recruitment and data collection took 24 months (2016 and 2017).
Statistical analysis
The description of the sample was made using means, standard deviations, and ranges for the continuous variables, and frequencies and percentages for the categorical variables. The internal consistency of each subscale was evaluated by calculating Cronbach’s alpha coefficients. To this end, the answers were recorded in the questionnaire to group them into three categories, in which a higher score implies a greater need: 1 = unfelt need, 2 = need felt but met, and 3 = need felt but unmet.
Results
Adaptation of the instrument
The four expert judges agreed to modify the syntax of the answer options. The original options “I have felt this need and I have been satisfied,” “I have felt this need but it has not been met,” and “I have not felt the need,” were replaced with: “I have felt this need and it has been met,” “I have felt this need but it has not been met,” and “I have not felt this need.”
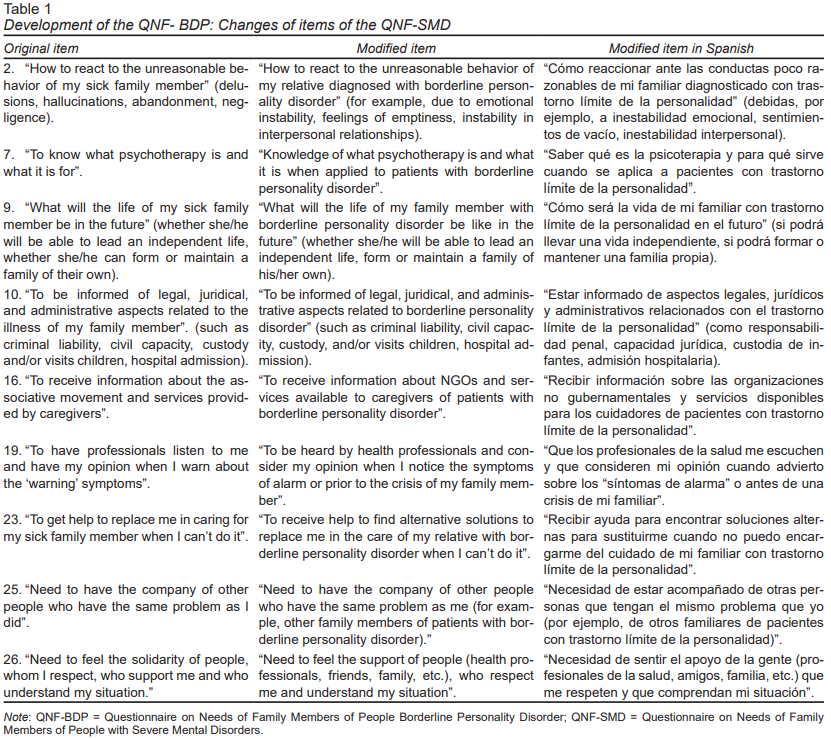
Table 1 presents additional changes to the items agreed by the expert judges. As can be seen, the instrument underwent very few changes, mostly in expressions, adding examples to specify situations in keeping with Mexican Spanish or according to the conditions of family members of patients with BPD (vs. a SMD in general).
Detection of needs and internal consistency
The total sample in this part of the study consisted of 80 IPCs of persons with BPD. We ended up with this sample after the invitation to participate in the study to 95 IPCs of persons with BPD; one of them refused to participate explaining that he did not need any help or service as IPCs, and 14 accepted to participate and initiated the questionnaire, but decided to withdraw from the study arguing that they did not have enough time to complete the questionnaire.
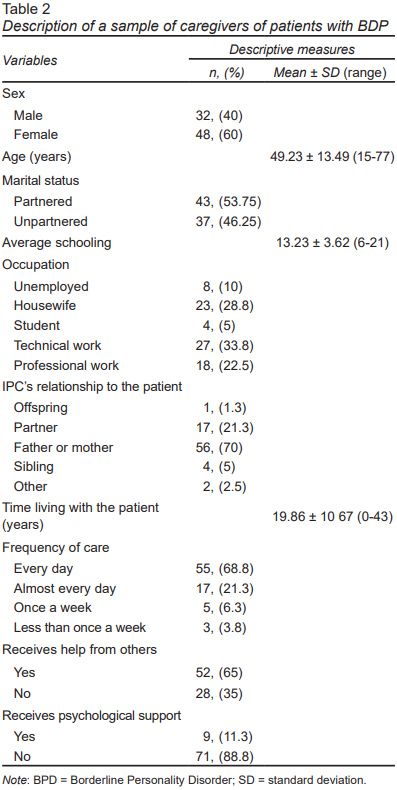
Table 2 presents the demographics of caregivers, showing that a high percentage are parents (70%) and take care of their family member with BPD on a daily basis (68.8%); while only 11.3% receive psychological support.
Cronbach’s alpha coefficients of the adapted questionnaire were: for the total score = .86; for the Knowledge/information subscale = .77; for the Instrumental support subscale = .78; for the Participation subscale = .63; and for the Personal support subscale = .74.
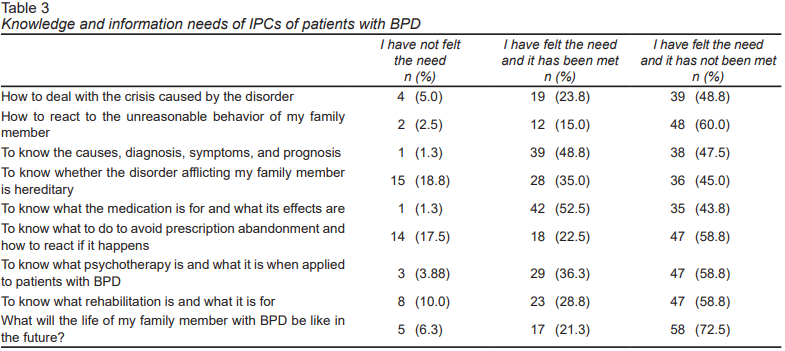
Table 3 shows the frequencies of the responses of the different needs for Knowledge/ information in the total sample. There is a predominance of unmet needs concerning Knowledge/information about: what the life of the family member with BPD will be like in the future (72.5%); how to react to the unreasonable behavior of the family member (60%); what to do to stop them from abandoning their medication (58.8%) and how to react if this happens (58.8%); what psychotherapy is and how it works when applied to patients with BPD (58.8%), what rehabilitation is and what is it for (58.8%), and how to deal with the crisis of the family member (48.8%). The main met needs were knowledge of: medication and its effects (52.5%) and the cause, symptoms, and prognosis of BPD (48.6%).
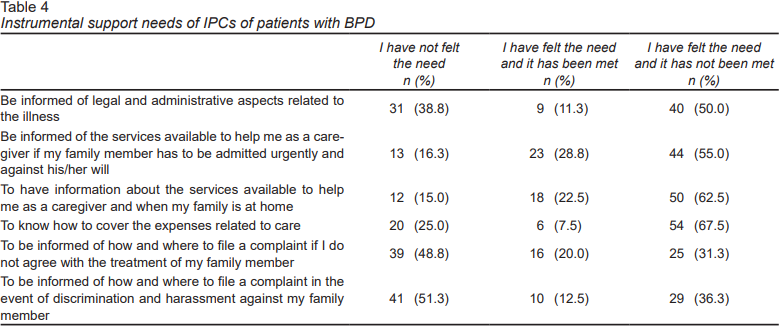
Table 4 presents the results of the section on Instrumental support. The most frequent unmet needs were knowing about: how to cover expenses related to the care of the family member with BPD (67.5%); services available to caregivers when they were not at home (62.5%), or when their relatives had to be admitted urgently against his/her will (55%), as well as regarding legal and administrative aspects related to the treatment of the illness (50%). Unmet needs included: being informed about how and where to file a complaint in the event of discrimination or harassment against the family member with BPD (51.3%) or if the IPC was dissatisfied with the treatment of his/her relative with BPD (48.8%).
Table 5 shows the results about Participation and personal needs. Regarding Participation, the most frequent unmet needs included: receiving information about support groups and services for caregivers (55%); being listened to by health professionals to give their opinions as caregivers during the evaluation of the family member with BPD (51.3%); and consulting with a professional (psychiatrist, psychologist) because of the stress of taking care of a relative with BPD (46.3%).
Finally, concerning the Personal needs of the IPC, the most frequent unmet need was for rest and a reduction of the feeling of responsibility in caring for a relative with BPD (47.5%), whereas the met needs were that professionals used words they could understand (58.8%) and to feel people’s support (45%). Needs that were not felt include: for professionals to consider the right of the IPC not to assume certain responsibilities regarding the treatment of BPD patients (52.5%); to receive help in finding an alternative solution for the care of the family member with BPD when the IPC is unable to do so (51.3%); and the need to have the company of other people who have the same problem (48.8%).
Discussion and conclusions
The version of the Questionnaire on the Needs of Family Members of People with Severe Mental Disorders (QNF-SMD) (Gómez et al., 2012), adapted to Mexican Spanish to assess the care needs of IPC of patients with BPD (QNF-BDP), demonstrated satisfactory internal consistency coefficients for the total score and for all its subscales, which were similar to those reported for the original version, with a total Cronbach’s alpha = .80 (Gómez et al., 2012), suggesting that this measure is reliable for clinical and/or research purposes in our population.
In our sample of IPCs of people diagnosed with BPD, the results in the area of Knowledge/information needs suggest the relevance of including, as part of the interventions for family members, information on the prognosis and likely outcomes of people with BPD; on how psychotherapy and rehabilitation works in these patients; as well as training in assertive, emotional self-regulation, and problem-solving strategies, which might allow IPCs to react more appropriately to the probable abandonment of medication and/or the unreasonable behavior of their relatives with BPD.
At the same time, the results regarding the needs of Instrumental support highlighted the importance of informing relatives of patients with BPD about financial aid programs and the means for obtaining them (for example, to reduce spending on medication through government health insurance that provides it free of charge – such as the “Seguro Popular” [Mexico’s People’s Insurance Scheme], which covers, among other things, the pharmacological treatment of depression, a very frequent comorbid diagnosis in BPD patients). This need has also frequently been detected in other samples of ICPs of patients with a SMD (Guillen, 2011). The care of a patient with BPD not only involves several costs in addition to medication, medical consultations, and recurrent hospitalizations, but also everyday expenses that may be significant in the case of patients with a high dysfunction level.
Finally, the Personal needs for rest and reduction of the sense of responsibility of the ICP is frequently expressed, which means the probable usefulness of incorporating a set of specific strategies to increase the professional and social support into interventions for family members, such as stress reduction, depression treatment, coping skills, problem solving, anxiety reduction, and adaptive emotional management (Hoffman et al., 2005). Along these same lines, Segurana & Bartel (2016) concluded that the care for patients diagnosed with BPD cannot be dealt with separately from the care for their caregivers. Providing adequate guidance and support based on specific needs prevents overload and other health problems, making it necessary to establish specialized intervention plans focused on the problems experienced by these primary caregivers.
One limitation of this study, which should be addressed in future research, is to evaluate other psychometric properties of the QNF-BPD, including its temporal stability (though a test-retest of the instrument, which could not be performed in this study since the participants were not available for a certain period of time). This would provide a more reliable evaluation of the positive changes that might occur with interventions designed to meet the needs of IPCs of patients with BPD in our context.
Additionally, the generalizability of the results should be taken with caution, given that the sample of the IPCs of people diagnosed with BPD included in the study comes from a specialized urban care center, where both IPCs and patients with BPD receive attention, and so could have less felt needs that have not been met. In other words, although it is highlighting the need for a comprehensive intervention for IPCs, the present picture may be better that the one which most caregivers face in contexts like ours.
Thus, the data obtained through the present study constitute a first step towards meeting the specific needs felt yet unmet by most IPCs of patients with BPD, including more specific psychoeducation objectives and therapeutic strategies for the development of emotional and cognitive skills.
The adapted version of the Questionnaire on the Needs of Family Members of People with Severe Mental Disorders (QNF-SMD) (Gómez et al., 2012), to identify felt and unfelt needs that may have been met or not by IPCs of patients with BPD (vs. a SMD in general) –the Questionnaire on the Needs of Family Members of People with Borderline Personality Disorder (QNF-BPD)–, is characterized by a satisfactory internal consistency and allows the opportunity to explore the particular needs of this population, including psychoeducation about BPD and its treatment, assertiveness training, stress management, and problem-solving.