Introduction
The stage of pregnancy in women is characterized by physical and psychological changes that lead to the development of positive or negative emotional responses towards the body image of the future mother. Body image is defined as the internal representation a person has of her body, regardless of what it really looks like, and consists of three components: 1. cognitive-affective, defined as the thoughts, beliefs, and feelings that a person may have regarding her body or a part of it, 2. perception, regarded as the accuracy with which the size and shape of the body is perceived in its entirety or a part of it, and 3. behavioral, meaning the actions people perform in order to check, alter, or conceal their bodies (Cash & Smolak, 2011).
There is increasing evidence that pregnant women worry about issues related to their body image and weight gain throughout the entire pregnancy process (Fahami, Amini-Abchuyeh, & Aghaei, 2018; Meireles, Neves, de Carvalho, & Ferreira, 2015a). It is estimated that approximately 50% of pregnant women report feeling dissatisfied with their bodies and their weight (Shloim, Hetherington, Rudolf, & Feltbower, 2015; Sui, Turnbull, & Dodd, 2013). Qualitative studies report that body image is a complex process and not fully understood, especially during the period of pregnancy, in which it has been noticed that pregnant women reflect a series of feelings and perceptions about body shape and size, including complete satisfaction, conflict, or a mixture of feelings of joy, lack of appreciation, and dislike of their bodies (Hodgkinson, Smith, & Wittkowski, 2014; Watson, Fuller-Tyszkiewicz, Broadbent, & Skouteris, 2015).
Likewise, it has been observed that dissatisfaction with the body image during pregnancy is related to adverse effects on the mother’s health such as depression and anxiety (Lee, Williams, & Burke, 2019; Roomruangwong, Kanchanatawan, Sirivichayakul, & Maes, 2017), including unhealthy eating behaviors such as binge eating, or intermittent fasting (Vartanian & Porter, 2016), and inadequate control of gestational weight gain (Hartley, McPhie, Skouteris, Fuller-Tyszkiewicz, & Hill, 2015). All these associated problems can affect the health of the fetus in the short- and long-term (Hartley, Hill, Bailey, Fuller-Tyszkiewicz, & Skouteris, 2018; Meireles, Neves, de Carvalho, & Ferreira, 2015a, 2015b). Moreover, this dissatisfaction with one’s body image can cause concern about recovering an adequate figure after childbirth, while failure to achieve this could trigger or aggravate the symptoms of anxiety and depression in the postpartum period (Silveira, Ertel, Dole, & Chasan-Taber, 2015). It is therefore important to have a tool to detect this body image disorder in this population.
Most studies that have evaluated body image in pregnant women have used body image scales designed for non-pregnant women (Bagheri et al., 2013; Hartley, McPhie, Fuller-Tyszkiewicz, Hill, & Skouteris, 2016; Shloim et al., 2015). However, since major changes occur in different parts of the body (such as the stomach, breasts and skin) during pregnancy, body image in pregnant women may differ from that of non-pregnant populations (Fuller-Tyszkiewicz, Skouteris, Watson, & Hill, 2013; Watson et al., 2015).
An instrument developed to evaluate negative and positive attitudes towards body weight gain in pregnant women has been identified: the “Pregnancy and Weight Gain Attitude Scale” (PWAS), which considers the evaluation of cognitive-affective and behavioral components of body image, and has acceptable reliability (Palmer, Jennings, & Massey, 1985), and construct validity (Kendall, Olson, & Frongillo Jr., 2001). In 2013, DiPietro, Millet, Costigan, Gurewitsch, and Caulfield (2003) evaluated the psychometric properties of PWAS in North American pregnant women, and Rousseau, Bouillon, Lefebvre, Séjourné, and Denis (2016) did so with pregnant women from France. The first study reported a reliability of .84, and the second a reliability of .70. It is worth mentioning that there is no version of the PWAS in Spanish nor has it been used in Latin American populations. It is therefore considered necessary to have a reliable, valid tool able to identify and measure attitudes towards body image in these populations.
In short, more research based on reliable measures is required to explore the body image component during pregnancy so that we can improve our knowledge of possible adaptation mechanisms. Although evidence exists that body image distortion problems are common in the Mexican population (Bobadilla-Suárez & López-Avila, 2014; Meza Peña & Pompa Guajardo, 2018), most of our knowledge about body image during pregnancy is drawn from studies conducted in other countries mainly developing ones. Accordingly, in order to improve the comparability of studies, it would be beneficial to evaluate body image with the PWAS in the Mexican population. The objectives of this study were therefore as follows: to adapt the Scale of Attitudes towards Pregnancy and Weight Gain to Spanish (referred from now on as PWAS-S); analyze its factor structure; verify the internal consistency of the factors; determine their second order factors and corroborate the proposed factor structure model in the Mexican population.
Method
Study design
A cross-sectional design was used.
Participants
Five hundred and twenty pregnant women over 18, with a single pregnancy, who were attending routine prenatal check-ups in the gynecology department of a public hospital in northeastern Mexico participated. Convenience sampling was used and the sample size was considered adequate according to the scale items and Likert format for exploratory factor analysis (Costello & Osborne, 2003).
Pregnant women with threatened miscarriages and those who had had cardiometabolic diseases (gestational diabetes, preeclampsia, hyperthyroidism, bulimia, or anorexia) were excluded.
Measurements
Personal data card
A registration card was used which included the sociodemographic (age, schooling) and obstetric data (weeks of gestation) of the participants.
Pregnancy and Weight Gain Attitude Scale (PWAS) by Palmer et al (1985). This scale was designed to assess the attitude of women in relation to weight gain during pregnancy in North American women. This scale consists of 18 items, 15 of which are related to attitudes and three to behavior. Answers to the items are formulated on a Likert scale with five response options (from 1 = strongly disagree, to 5 = strongly agree).
The total score is calculated by inverting nine negative items (1,3,4,9,12-17). Scores range from 18 to 90 points, with higher scores indicating a more positive attitude to weight gain. The PWAS has shown psychometric properties and indices with acceptable internal reliability for the Spearman Brown coefficient with a value of .67 (Palmer et al., 1985), as well as in the North American population, with Cronbach’s alpha from .75 to .84 (DiPietro et al., 2003) whereas in the French population, an alpha of .70 has been reported (Rousseau et al., 2016).
The English version (DiPietro et al., 2003) proposes a four-factor structure with 16 items: positive image of pregnancy (items 6,7 and 11), negative image of pregnancy (items 1,9,12,13,14 and 15), indifference towards weight gain (items 5,8,10 and 18), and restrictive behaviors in response to weight gain (items 3.16 and 17). Items 2 and 4 were excluded.
Procedures
This study was conducted in the period from April 2016 to July 2017, in two stages: cross-cultural adaptation to determine the linguistic validity of the scale, and verification of psychometric properties. In order to carry out the cross-cultural adaptation, five steps were followed: initial translation, translation synthesis, retranslation, review by a committee of experts and preliminary test (Beaton, Bombardier, Guillemin, & Ferraz, 2000). Before conducting the preliminary test on 45 pregnant women, experts evaluated each item in the translated versions using four criteria (semantic, idiomatic, experiential, and conceptual equivalence).
Lastly, the internal validity and construct validity of the scale in the Spanish version was explored; the scale was self-administered by 520 pregnant women. Data collection was undertaken by previously trained health personnel, the average response time by participants being 12 minutes.
Statistical analysis
The dimensional structure was first determined by exploratory factor analysis of the main components using the Varimax rotation method. Using the scores of the factors calculated by the simple addition of items, a second order exploratory factor analysis was performed. The same methods and number of fixed factors were used according to Kaiser’s criteria. Internal consistency was estimated using Cronbach’s alpha coefficient. High ≥ .70, adequate ≥ .60 and low values < .60 (Cronbach & Shavelson, 2004) were considered.
Secondly, the models of factors correlated and ranked by confirmatory factor analysis were contrasted. The Generalized Least Squares method was used to estimate the discrepancy function, parameters, and fit indices. Seven fit rates were considered: discrepancy function (DF); chi-square test (χ2); coefficient between chi-square and its degrees of freedom (χ2/gl); population non-centrality parameter (PNCP), Steiger and Lind’s root mean square error of approximation (RMSEA); Jöreskog and Sörbom’s goodness of fit index (GFI); and its adjusted version (AGFI). The following values are considered to have a good fit: p of χ2 > .05, fd and χ2/gl < 2, PNCP < 1, RMSEA < .05, GFI > .95 and AGFI > .90; while those given below are regarded as having an adequate fit: p of χ2 > .05, DF and χ2/gl < 2, PNCP < 2, RMSEA < .08, GFI > .85 and AGFI > .80 (Landero Hernández & González Ramírez, 2006). Statistical calculations were performed in the SPSS and AMOS 7 program.
Ethical considerations
The procedures used in this study adhered to the principles of the Declaration of Helsinki (World Medical Association, 2001) and the regulations of the General Health Law on Health Research Matters (Secretaría de Salud, 1987). Participants signed an informed consent form and the confidentiality and security of the information and privacy of the participants were protected at all times.
Results
The mean age of the participants was 23.56 ± 5.89 years, with an average of 33.20 ± 6.69 weeks of gestation, and an average monthly income of 4448.57 ± 4958.370.
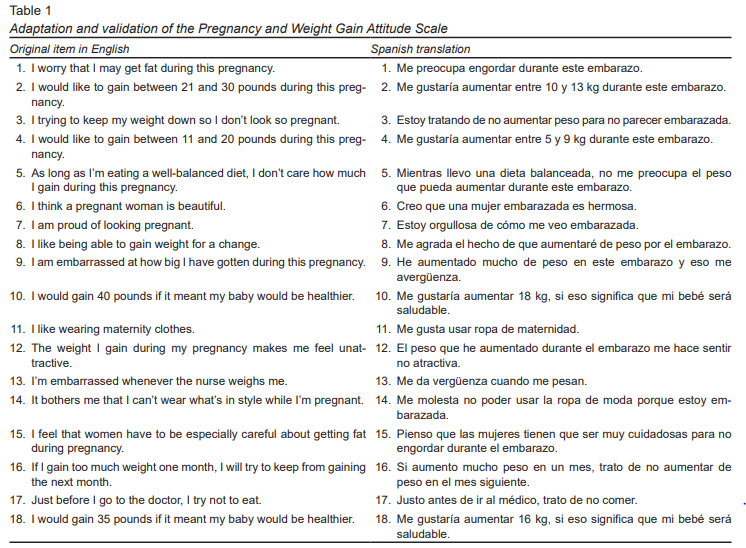
The adaptation and translation of the PWAS-S was carried out by a group of experts. Changes included the following adaptations: weight was converted from pounds to kilograms, and weight gain was translated as weight increase (Table 1).
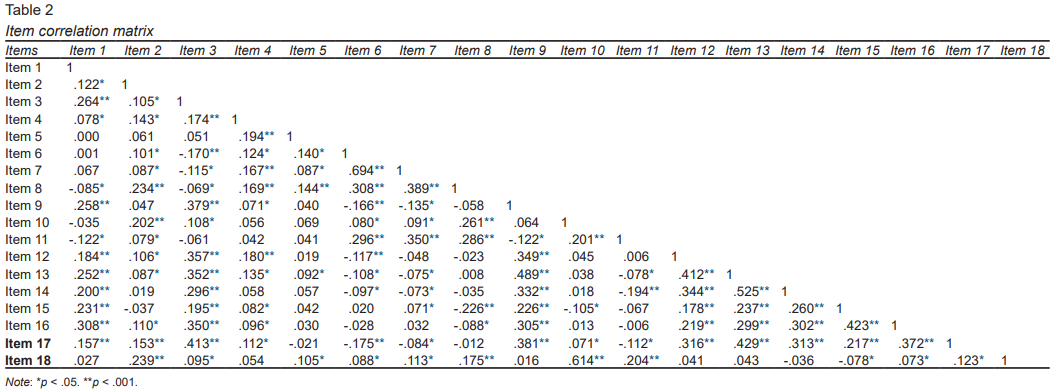
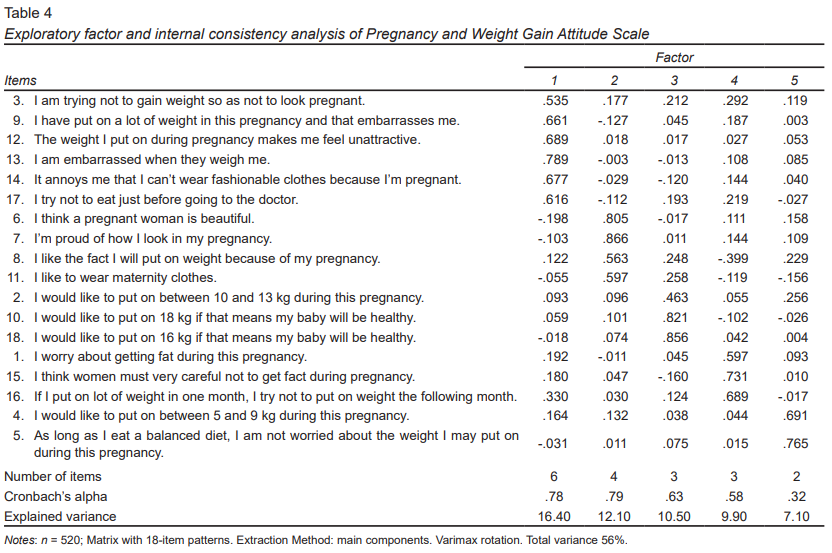
As observed in Table 2 , both positive and negative correlations were found, which were usually statistically significant between the items. Regarding the results of the exploratory factor and internal consistency analysis, five components were defined and these explained 56.04% of the total variance of the 18 items. After rotating the component matrix by the Varimax method, five factors were confirmed: 1. factor one “Negative attitude towards the increase of gestational weight,” comprising six items; 2. factor two “Positive body image,” consisting of four items; 3. factor three “Gestational weight control,” with three items; 4. factor four “Concern over the increase in gestational weight,” consisting of three items; and 5. factor five “Restrictive behavior in response to gestational weight,” consisting of two items. Most items show loads over .50.
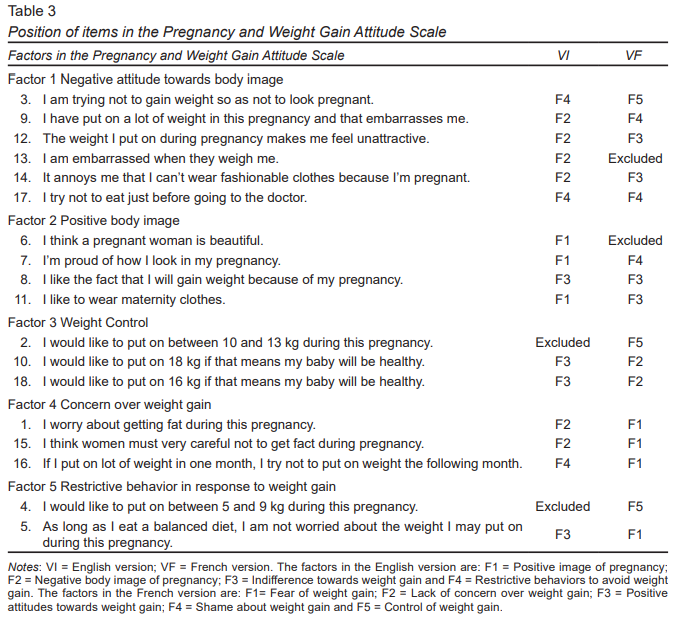
The assignment of the names of the factors followed the dimensions proposed by Cash and Smolak (2011), and the coincidence of the items grouped together in the English and French version (Table 3). Four factors were explored in the English version, whereas in the French version, five factors were examined, as in the Spanish version.
The total internal consistency of the scale was .78 and factors one and two had the greatest internal consistency (Table 4).
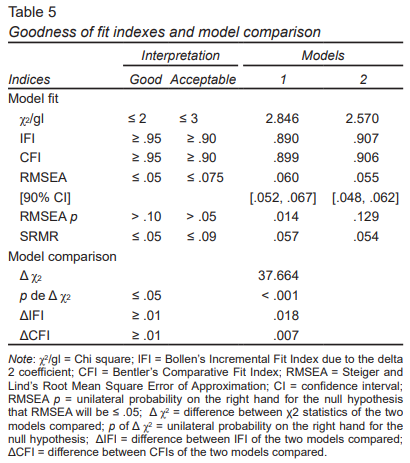
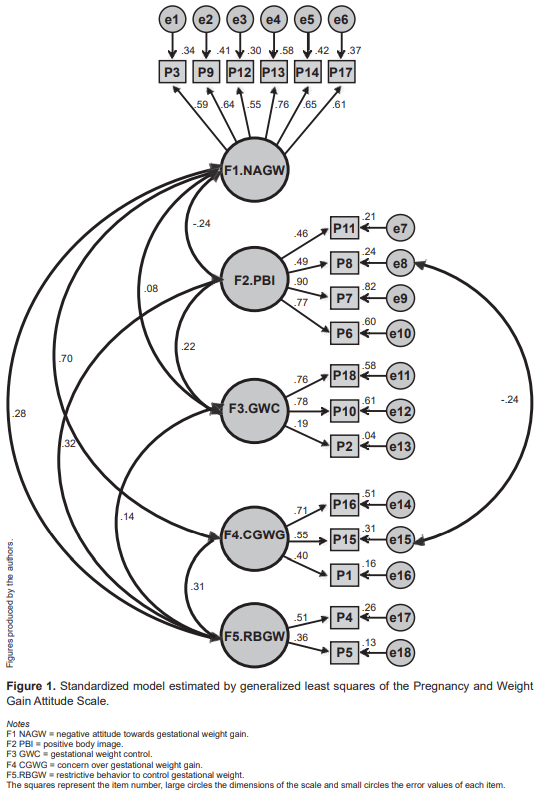
The five-factor model produced by the exploratory factor analysis was contrasted in the confirmatory factor analysis. Model two showed adequate fit rates: χ2/gl = 2.57, IFI = .90, CFI = .90, RMSEA = .05 (90% CI [.048, .062], p = .12), SRMR = .05 (Table 5) with 18 items and nine correlations.
Figure 1 shows the standardized regression coefficients between the factors, which ranged from -.22 to .88, as well as the correlations of the factors and items which ranged from .17 to .88.
Discussion and conclusion
The results indicated that this instrument has good psychometric properties and can be recommended as a simple, valid tool for assessing attitudes towards body image in Mexican women during the period of pregnancy in health centers or primary care clinics.
Factor analysis confirmed five factors (negative attitude towards the increase of gestational weight, positive body image, control of gestational weight, concern about gestational weight, and restrictive behavior in response to gestational weight) through 18 items. The aforementioned dimensions explain 56% with adjustable indices, which is higher than the values in the model proposed by DiPietro et al. (2003) and Rousseau et al. (2016).
The dimension called “negative attitude towards increased gestational weight” reported further explanation of the variance. This dimension includes six items, four of which coincide with the negative body image dimension of pregnancy proposed by DiPietro et al. (2003). Dimension two, called “positive body image,” includes four items, three of which coincide with the sphere of positive body image of pregnancy of the model proposed by DiPietro et al. (2003). These two dimensions coincide with the cognitive-affective component of the body image concept proposed by Cash and Smolak (2011). It is worth mentioning that these two aspects of body image attitudes can impair postpartum weight control and that negative attitudes can continue during the postpartum period (Phillips, King, & Skouteris, 2014; Silveira et al., 2015).
Regarding dimension three, called “gestational weight control,” which includes three items, two items coincide with the sphere of indifference towards weight gain in the model proposed by DiPietro et al. (2003) and the item “I would like to gain between 10 and 13 kg during this pregnancy” was excluded in the analysis of the model designed by DiPietro et al. (2003). However, this item was included in the sphere “lack of concern about weight gain” in the model proposed by Rousseau et al. (2016). Weight control during pregnancy may be adequate or inappropriate, and will depend on the perception, attitudes, or dissatisfaction with the body image of the pregnant woman (Meireles et al., 2015b; Shloim et al., 2015).
Continuing with the description of the dimensions of this study, dimension four, called “concern about weight gain” includes three items, coinciding with the sphere of fear of weight gain in the model proposed by Rousseau et al. (2016). This dimension coincides with the concern over appearance in pregnancy scale, given that one of the items asked whether women had restricted the amount of food they ate during pregnancy in order to feel thinner (Nagl, Jepsen, Linde, & Kersting, 2019).
In dimension five, called “restrictive behavior towards gestational weight,” which includes two items, item four “I would like to put on between 5 and 9 kg during this pregnancy” was not contemplated in the analysis of the model proposed by DiPietro et al. (2003), although it was included in the weight gain control sphere in the model proposed by Rousseau et al. (2016). Item five, “as long as I eat a balanced diet, I am not worried about any weight I might gain during this pregnancy,” was included in the dimension of indifference towards weight gain in the model proposed by DiPietro et al. (2003) and in the dimension of fear over weight gain proposed by Rousseau et al. (2016). These dimensions coincide with the behavioral component of the concept of body image, in other words, the actions people perform with the aim of checking, altering, or concealing their bodies (Cash & Smolak, 2011). These statements coincide with other scales, where women engage in certain eating behaviors to enhance their physical appearance (Watson, Fuller-Tyszkiewicz, Broadbent, & Skouteris, 2017).
The model used in this study shows that item eight “I like the fact I will gain weight during pregnancy” has a negative relationship with item 15 “I think women should be very careful not to gain weight during pregnancy.” This relationship illustrates the idea that pregnant women can have a positive attitude towards weight gain during pregnancy and at the same time take care not to increase more than the recommended weight. These positive feelings are manifested in first-time mothers (Bergbom, Modh, Lundgren, & Lindwall, 2017).
As regards internal consistency, the pregnancy and weight gain attitude scale is considered a reliable tool for measuring the construct, because internal consistency values and fit rates were adequate, and similar to those in the study proposed by DiPietro et al. (2003) and Rousseau et al. (2016). The dimensions of the scales report acceptable values of internal consistency, with the exception of dimension four and five. These dimensions report low values from .32 to .58, which can be attributed to the number of corresponding items in each dimension.
Limitations of this study include failure to perform criterion validity, which indicates the degree to which questionnaire scores correlate with other questionnaires measuring the same trait or variable. At present, a standard instrument has yet to be established to measure body image distortions (Meireles et al., 2015a).
From the statistical point of view, it is concluded that the Scale of Attitudes towards Pregnancy and Weight Gain (PWAS-S) in its Spanish version reports acceptable construct validity and reliability, indicating that it can be used in Mexican pregnant women over 18.
It is important for health professionals involved in prenatal care and trained in mental health to consider the assessment of body image during pregnancy, in order to improve prenatal care in relation to the body changes that normally occur during this period. This will enable pregnant women to accept changes in their appearance.
The above is proposed, because in recent years, there have been reports that most women react negatively to the changes in body appearance characteristic of pregnancy (Lee et al., 2019; Meireles et al., 2015a), although a minority of pregnant women perceive changes in the body’s appearance during pregnancy as being positive (Erkaya, Karabulutlu, & Calik, 2018; Harrison, Obeid, Haslett, McLean, & Clarkin, 2019). This dissatisfaction with their bodies may lead women to adopt eating behaviors and emotional states that can create problems with the recommended weight gain during pregnancy (Hartley et al., 2018; Roomruangwong et al., 2017) and jeopardize the health of the mother and the fetus in the short- and long-term. The consequences of failing to achieve the recommended weight, coupled with the eating and emotional disorders that may occur during pregnancy, show the importance for primary health care professionals of having reliable tools to detect attitudes towards body image.
Funding
None.
Conflicts of interest
The authors declare they have no conflicts of interest.