Introduction
Children with mental disorders generally depend on family attention and support since they require more intensive care and need help, time, and supervision in daily activities (administration of medication, treatment routine, coping with problematic behaviors, school activities, and support in stigmatizing situations, among others) (Campelo, Costa, & Colvero, 2014; Buriola, Vicente, Zurita, & Marcon, 2016; Farias, Lima, Ferreira, Cruzeiro, & Quevedo, 2014).
Mental disorders can result in losses in various areas of development including interpersonal relations and social insertion, which may generate problems of family functioning and dynamics (de Souza Nunes, & Werlang, 2008). Another important grievance concerns academic performance and learning difficulties, which will also have an impact on all areas of development (de Magalhães Monteiro & Santos, 2013; Pereira, et al., 2015; Petrucci, Borsa & Koller, 2016).
The family is the first environment that helps the child in the process of socialization by teaching, counseling, and providing affection, values, and physical and emotional care; it is also the major source of social support of an individual (Minuchin, 1990). It is within this context that daily activities take place and can promote independence, autonomy, the use of resources, and the development of interpersonal relations (Short, Eadie, Descallar, Comino, & Kemp, 2017; Cid, 2015; Flores, Salum, & Manfro, 2014). Despite the importance of the family, there is a scarcity of studies focusing on the family environment of these children and on analyzing its different, positive or negative, conditions that may interfere with child development and family functioning.
The daily routine of the family of a child with a mental disorder is altered, with a frequent reduction of the participation in events and changes in social habits and in the relationship among family members. Consequently, there may be a social isolation of the child and commonly an overprotective attitude on the part of the parents, which limit their participation in a series of activities (Vicente et al., 2013; Hock & Ahmedani, 2012; Gomes, Martins & Amendoeira, 2011). This is also due to the behavioral problems of the children, the difficulty in dealing with them, and the feeling of shame experienced by the family (Day et al., 2018; Green et al., 2016).
Thus, the family environment may represent a protective factor (by offering support and opportunities) or a higher risk (by limiting social participation and activities) for child development. Within this context, an interaction between parents and children plays a fundamental role because, within the bioecological model, this context is interconnected with all other contexts in which the child participates (Wright, Masten, & Narayan, 2013; Bronfenbrenner, 2011).
Children with mental disorders have behavioral and/or emotional problems, with difficulty in social relations and in following norms and rules, with functional losses regarding autonomy and daily life (Dumas, 2011). Boys are more affected, with hyperactivity symptoms predominating among them. Several studies have reported that about 3% to 7% of these children are of school age and one of their more significant types of impairment involves the activities related to learning, which are interlinked with all areas of development (Belli, Muszkat, & Cracasso, 2015; Polanczyk, Salum, Sugaya, Caye, & Rohde, 2015; Ercan, Bilaç, Özaslan, & Ardic, 2016; Hillen & Gafson, 2015; Kato, Yanagawa, Fujiwara, & Morawska, 2015).
Depending on the attitude of the parents or other relatives living in the same environment, the presence of a person with a mental disorder may increase or reduce the family interactions (Green et al., 2016). Thus, the approach can be seen as a form of coping with adversity, becoming established as a protective factor (Rolland, 2016; Wang, & Zhao, 2012). It is known that a family with healthy functioning has a positive influence on child development by promoting prosocial behaviors (Renzaho, Mellor, Mccabe, & Powell, 2013).
On the other hand, the family’s approach to the child may be seen as a condition of risk for development. The child with mental disorders requires greater attention and care with constant supervision and at times is not stimulated in terms of the process of autonomy, becoming a source of care overload, as well as a target of overprotection by the parents or caregivers (Buriola et al., 2016; Flores et al., 2014). The mental disorders of children cause significant changes for the family either because of their particular characteristics or because of the need to reorganize the environment in order to meet the child’s requirements.
The objective of the present study was to determine which environmental resources are offered to children with mental disorders by their family and how they correlated with the family functioning.
Method
Participants
This is a cross-sectional study which conducted between August 2016 to April 2017, with 33 caregivers (parents or grandparents) of children, who attended at the ambulatory service of psychiatry of a general hospital in Ribeirão Preto, São Paulo, Brazil. Sample size was calculated based on the total sampling, made up by 51 patients in total.
Inclusion criteria were self-report of being the child’s primary caregiver and 18 years or older. The child should be between 6 and 12 years old and diagnosed with a mental disorder by psychiatrist. Exclusion criteria were caregivers with mental disorders and children with other health conditions that could interfere with family functioning and offer of resources, as reported in the literature (Ribeiro, Vandenberghe, Prudente, Vila & Porto, 2016; Macedo, Silva, Paiva, & Ramos, 2015).
The majority of participants/caregivers were mothers (78.8%), followed by parents (15.2%) and grandparents (6.1%). The mean age was 37.6 years (SD = 8.6), and 87.9% of respondents identified themselves as the primary caregiver of the child.
Instruments
Sociodemographic questionnaire
This questionnaire was constructed by the researchers with the purpose of characterizing families; it contains 25 questions about personal data and socioeconomic conditions (Associação Brasileira de Empresas de Pesquisa-ABEP, 2014).
Family Adaptability and Cohesion Evaluation Scale, version IV (FACES IV)
This scale, which is used to measure family cohesion and flexibility, was elaborated by Olson (2008) and adapted to Brazil (Santos, Bazon, & Carvalho, 2017; Santos, Bazon, Carvalho, Minetto, Crepaldi, & Boing, 2013). The scale contains 42 items divided into six main subscales: two of them balanced (cohesion and flexibility) and four unbalanced (disengaged, enmeshed, rigid and chaotic ‒ extreme conditions of cohesion and flexibility), and includes 20 additional items divided into two complementary subscales ‒ communication and family satisfaction (10 items each). In the construct of the instrument, cohesion refers to emotional/affective bonds, independence among family members, limits and decision making, and flexibility refers to the ability of family members to change the family structure, roles, and rules in the presence of adversities. The instrument consists of a series of statements to be answered according to a Likert-type 5-point scale. The results can be calculated based on the combination of scores and percentiles of the balanced and unbalanced scales (ratio), allowing to differentiate between healthy families (functional, ratio ≥ 1) and unhealthy families (dysfunctional, ratio < 1). For the balanced and complementary subscales, the higher the score, the healthier the family. For the unbalanced subscales, the higher the score, the greater the family dysfunction. Reliability studies according to Olson (2011) and in the present study with Cronbach’s Alpha of .83.
Family Environment Resources Inventory (RAF)
This is an instrument based on the bioecological concept of development that assesses the resources of the family environment considering three domains: resources that promote proximal processes, activities that stabilize family life, and parental practices that promote the family-school relationship (Marturano, 2006). The inventory is applied in the form of an interview organized into ten topics: recreational activities in the home/neighborhood, family outings, programmed and regular activities, joint home activities with parents/persons responsible, availability of toys, newspapers, magazines and books, school support and supervision, organization of schedules, and family gatherings for routine activities. The result is given by the score for each topic. The study of the instrument presented satisfactory reliability index between .70 to .84 of Cronbach’s alpha (Marturano, 2006), which was confirmed in the present study (α = .84).
Procedure
Participants were approached in the waiting room of the psychiatry service and referred to the doctor’s office to be informed about the details of the investigation, to give written informed consent, and to answer the questionnaires individually.
The study protocol was approved by the Ethics Committees for Research on Human Beings of the Nursing School of Ribeirão Preto and of the University Hospital of the Faculty of Medicine of Ribeirão Preto, University of São Paulo (CAAE: 56525416.2.0000.5393). All participants gave written informed consent to participate in the study.
Statistical analysis
The data were organized and the analyses were performed using the SPSS software, version 24.0. The frequency and percentage of the categorical variables were then calculated, together with the central tendency measures for the numerical variables. The Spearman correlation test was applied to determine the associations between family functioning (FACES IV) and the availability of resources in the family environment (RAF).
Results
A total of 33 caregivers (parents or grandparents) of children, aged between 6 to 12 years old (M = 8.3, SD = 1.86); 69.7% were boys and 30.3% were girls; 78.8% frequented school. The most frequent diagnoses were: attention deficit hyperactivity disorder (39.4%), and autism spectrum disorder (39.4%), followed by oppositional defiant disorder (12.1%), and schizophrenia (12.1%). Psychiatric comorbidities were present in 24.2% of the patients. In relation to other caregiver information, Table 1 presents such results.
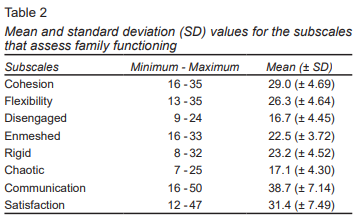
The results of family functioning (FACES IV) indicated that 12.1% (4) of the families were dysfunctional. The mean balanced cohesion score was higher than the flexibility score, and in the unbalanced subscales the highest means were observed for the enmeshed (excessive approximation between members with little opportunity for privacy) and the rigid (strict adherence to norms and rigidly defined functions) features (Table 2).
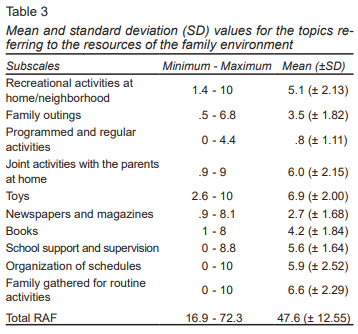
The offer of toys, family gatherings for routine activities, and joint home activities with the parents were the resources most frequently offered by the families, whereas there was little offer of programmed and regular activities (extracurricular activities) (Table 3).
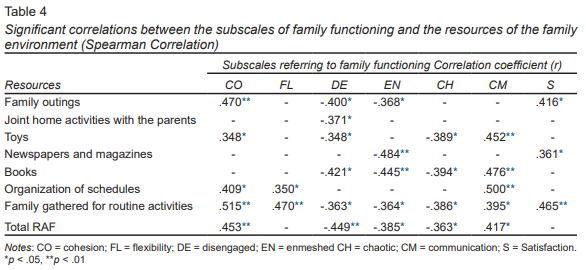
The correlation results are presented in Table 4. The subscales of recreational activities at home/neighborhood, programmed and regular activities, school support, and supervision did not correlate with family functioning. The strongest correlation detected was family cohesion and family gathered for routine activities (r = .515). The scales associated with family dysfunction (disengaged, enmeshed, and chaotic) always showed negative correlations with the availability of resources in the environment. Rigidity of family norms and rules was not correlated with the topics investigated by the RAF (Table 4).
Discussion and conclusion
The main objective of the present study was to evaluate the functioning of families who have a child with a mental disorder and to determine whether they offer resources to their children within the family environment. Our attempt was thus to determine an association between these variables.
Regarding family functioning, analysis of the results obtained revealed that most families (87.9%) showed good functioning despite the presence of a mental disorder of a child.
On the basis of these results and of the analysis of the mean scores for the FACES IV subscales, we may infer that a possible strategy found by the family in order to cope with the disease and the treatment of the child is related to the strengthening of ties among the family members (cohesion), at times with some enmeshed relationships. Adherence to family rules and a strict definition of the roles of the family members (Rigid subscale) may also be used as a strategy for the maintenance of the health of the family group.
Similar results were obtained in a previous study that observed that the families of children with mental disorders showed higher cohesion scores and exhibited more frequently a functioning of the enmeshed type when compared to the families of children with no diagnosis of psychopathologies (Pepe, Tortolani, Gentile, & Di Ciommo, 2015). This study reported that families with the presence of a psychopathology showed more chaotic-enmeshed and flexible-enmeshed family typologies, indicating a tendency of these families to enmeshment of the relationships.
Conversely, another study detected that the presence of children with behavioral problems is associated with less effective family functioning (Jellett, Wood, Giallo, & Seymour, 2015; Sikora et al., 2013).
The present results are also similar to those obtained in a study of adolescents with schizophrenia, which reported that most of the families showed healthy functioning (Wiguna et al., 2015). The present authors, however, detected a higher percentage of families defined as dysfunctional (24.4% compared to 12.1% in the cited study). This discrepancy may be due to a variation of age (adolescents vs. children) and to the difference associated with the mental disorder (schizophrenia vs. various mental disorders), or also due to the cultural diversity of the contexts within which the studies were conducted.
Demographic variables may explain variations of cohesion in the families of children with different mental disorders. The educational level of the parents and the family income have been previously pointed out as predictors of cohesion in the presence of this condition (Rieger & Mcgrail, 2013).
When compared to other Brazilian studies conducted on clinical samples, the present results concerning the resources of the family environment were in general slightly better than those observed among children with learning problems, except for data regarding the organization of schedules for routine activities (D’Avila-Bacarji, Marturano, & Elias, 2005). In addition when compared to data obtained for a sample with behavioral problems the present results were similar or better, except for programmed and regular activities (Ferreira & Marturano, 2002).
A study conducted on children with cerebral palsy detected higher values for different resources, except for three topics for which it detected similar or higher values than the present ones: organization of schedules (5.9 in both studies), school support and supervisions (5.6 in this study and 4.5 in the cited study) and family gathered for routine activities (with values of 6.6 in the present study and of 6.5 for children with cerebral palsy) (Morilla, Caldas, Scarpellini, & Santos, 2017). These divergences in samples from the same sociocultural context may indicate that mental health problems place the children in a more vulnerable condition regarding development than physical health problems or impaired physical/motor development, as is the case for cerebral palsy.
We should consider differences not only between sample profiles, but also in the form of conducting the interview in order to respond to the inventory. Also, it is important to remember that the studies were conducted at different times (10 years of difference), with increased discrepancy between samples. The profile of the children and of the mental disorders changed a long time, with the advancement of society and with new discoveries in the area of mental health and other related sciences.
The bioecological conception of development (the approach at the basis of the construction of the RAF instrument) emphasizes the importance of the replication of investigations that might reaffirm the findings of previous studies, pointing out the stable elements of development as well as the changes that occur over various generations (Bronfenbrenner, 2011). The RAF instrument itself was constructed in order to identify risk and protective factors in the family environment, although it did not incorporate the technological changes and the new resources offered over time to children.
Although various resources may be present in the homes of the families investigated, the programmed and regular activities (extracurricular experiences) are those least cited. In general, these activities are considered to be important contexts for development in view of the diversity of experiences that they provide, such as interaction with peers and with non-family adults, and the contact with rules and routines differing from those experienced at home and in school. The benefits have been pointed out, especially regarding academic engagement and performance and the development of prosocial behavior (Hughes, Cao, & Kwok, 2016; Pereira et al., 2015).
The literature indicates that practicing sports, having responsibilities in the home routine, and having at least one parent involved in leisure activities (community activities, sport or a hobby) are conditions more present among adolescents considered to be healthy or free of psychiatric disorders, possibly representing protective factors against mental disorders (Borkum et al., 2017).
At this point, we should consider the fact that the present study showed that most children frequented school, although a good part of them were outside the educational system, excluded from one more context in which the social interactions represent a key element for the development of different skills.
In addition, several investigations have indicated that social environments, such as the family, peer groups, school, and neighbors, are associated with better results in development. In particular, the family context and the groups of friends have been shown to be protective factors for child development (Wlodarczyk et al., 2017; Pereira et al., 2015).
In this respect, the present findings indicate a predominance of home activities with lower scores (which implies a lower occurrence) for activities in the neighborhood and outside the home (extracurricular activities and outings), with a consequent increase in the amount of time the relatives devote to these children (Sikora et al., 2013). It is possible that, due to the behavioral characteristics of the children (a predominance of ADHD and ASD), the parents do not feel encouraged to expose their child to environments outside the home. We should also consider the stigma created by the mental disorder, which inhibits the family regarding the search for spaces where social interaction with peers and adults might occur (Wlodarczyk et al., 2017). Activities that permit interaction with other people are fundamental for child development (Bayer et al., 2011).
Regarding the associations between family functioning and the resources of the family environment, the dimensions favorable to family functioning such as cohesion and communication showed positive associations with different family resources, in agreement with the results of a study on children with cerebral palsy conducted with similar objectives (Morilla et al., 2017). Conversely, the unbalanced cohesion extremes (related to the disengaged and enmeshed subscales) showed negative correlations with family resources.
The associations between environmental resources and unbalanced dimensions (including the chaotic subscale) clearly show that a problematic family dynamics reduces the possibility that the child will have materials and activities that could be of benefit for his development, strengthening his abilities and minimizing the effect of the risks due to the presence of a mental disorder.
Several studies have indicated that adversities during childhood have proved to be associated in a negative manner with family cohesion and flexibility. However, when family functioning is well adapted its members can develop in a satisfactory manner (Oshri et al., 2015; Muniz, Silver, & Stein, 2014). We may infer that, despite the presence of a mental disorder that may trigger a series of difficulties for both the child and the family, the families that establish affective closeness among its members with good cohesion and that have good communicative skills are able to offer more stimuli to the child, thus becoming promoters of development.
In general, belonging to a family with problematic functioning seems to increase the risk of maladapted development since these families are unable to provide resources or opportunities that may stimulate the development of its members. Growing up within adverse family contexts may impair psychosocial and emotional development and may frequently have an impact on future mental health (Luecken, Roubinov, & Tanaka, 2013).
On the other hand, the study contributes by indicating that aspects such as family cohesion and communication are favorable to development when they are strengthened. Future research directions should investigate how the type of mental disorder of the child interferes with the offer of resources by the family and focus on the variability of the functioning profile according to the type of psychopathology.
It is also important to understand the perception of the family about the activities and materials that may help children with mental disorders to develop different types of competence. In addition, investigations are needed in order to understand the processes by which the offer of resources and a healthy family dynamic may act as promoters of the development of the child.
The presence of mental disorders is not always associated with family dysfunction, although it seems to have some impact on the type of resources and activities the family offers to the child, especially giving the child the opportunity to participate in diverse social contexts. Affective closeness between family members and communicative skills seem to favor the greater variety of resources and activities to which the family exposes the child. The types of activities and the materials offered by the family may possibly vary according to the characteristics of the psychopathology.
Limitations
The present study has some limitations both regarding the possibility of generalization of its results by including a restricted group of participants and regarding the strategy used to investigate the resources of the family environment, since the instrument was developed for the Brazilian context and was not updated to incorporate new resources that may be available (electronic equipment and the internet).
Funding
This study was partially funded by CAPES - Comissão de Aperfeiçoamento de Pessoal do Nível Superior (Nº 33002029016P9).
Conflict of interests
The authors declare they have no conflicts of interest.
Acknowledgements
We are grateful to all families and to the team of the Service of Child and Adolescent Psychiatry that contributed to the study. We also wish to thank the research collaborators who helped with data collection. We thank CAPES (Comissão de Aperfeiçoamento de Pessoal do Nível Superior) for a Postgraduate fellowship granted to the senior author.