Background
The Official Standard for “front-of-package labeling” for frequently consumed processed foods was launched in an attempt to reduce obesity in Mexico (Secretaría de Salud [SSA], 2020). This involves the inclusion of octagonal labels placed in the top right-hand corner of processed foods indicating excess calories, sugars, saturated fats, trans fats, and sodium in the labeled products (SSA, 1998).
The recent National Health Survey (SSA, INSP, & INEGI, 2018) reported a prevalence of up to 86% of overweight and obesity based on the body mass index (BMI). At the other extreme, eating disorders (EDs) constitute the third most frequent and lethal chronic disease in children and adolescents. A prevalence of 1.3% was found (1.9% in females and .8% in males) in a small proportion of adolescents who participated in the ENSANUT 2012. The most frequent risky eating behaviors in Mexican adolescents were concern about weight gain, overeating, and losing control over what they eat.
The World Health Organization (WHO) has recommended the inclusion of front-of-package labeling. The aim is for consumers to be able to more easily identify foods considered “unhealthy,” thus changing their behavior, on the assumption they will choose healthier foods.
In European countries where actions similar to front-of-package labeling have been implemented, no significant evidence has been found on the decrease in consumption of these products, nor have the data indicated that the frequency of obesity based on body mass index decreased. However, a higher rate of psychiatric problems such as anxiety and depression related to the feeling of guilt over consuming these labeled products was observed (Figure 1).
This type of policies targets marginalized populations. But what about the group of patients suffering from eating disorders? Several studies have demonstrated a correlation between food insecurity and the prevalence of eating disorders. A study conducted in San Antonio, Texas, found that 17% of the most food insecure children met the diagnostic criteria for binge eating disorder (Becker, Middlemass, Taylor, Johnson, & Gomez, 2017; Nicholls, Devonport, & Blake, 2016). Weight loss interventions are clinically contraindicated in people suffering from an eating disorder (Hunger, Smith, & Tomiyama, 2020). Implementing this type of policy in populations with a higher risk of having an eating disorder, and who also lack access to treatment, is not advisable (Storcksdieck Genannt Bonsmann & Wills, 2012).
Likewise, in patients with a genetic predisposition, the distorted thinking and/or obsessive behaviors caused by these warnings on food packaging can trigger the development of an eating disorder.
The purpose of this article is to review the literature on front-of-package labeling of foods as a means of combating obesity in Mexico and other countries, to review the stigmas surrounding obesity and the potentially negative impact on diseases such as eating disorders.
Method
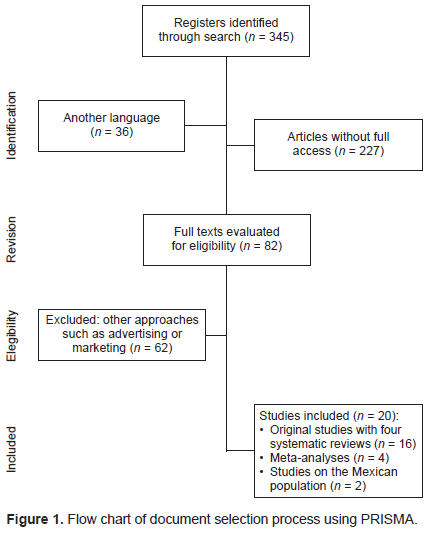
A search was conducted in PubMed and academic Google to include medical, marketing, and economics articles. It was an umbrella search (including systematic reviews and meta-analyses) of articles published until January 2021 on consumption, preference, perception, and behaviors related to food labeling. Studies in languages other than English, Spanish, and French were excluded. The search strategy was to use the following terms in English (food labeling OR front-of-package nutrition labeling) AND (meta-analysis OR meta-analyses) AND (obesity AND Weight control AND Eating disorders) AND (consumer preferences). Data searching, filtering, and data analysis were performed by independent researchers (CA and FG). Emails were sent to the authors of national studies, who reported that studies on groups of patients with eating disorders in Mexico have not been conducted. Approval by the ethics committee was not requested since this is a bibliographic review article.
Results
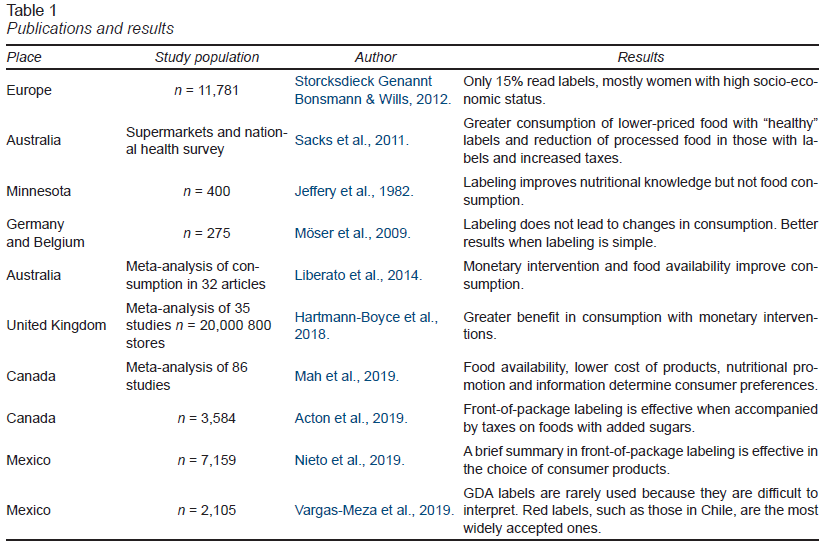
Three hundred and forty-five studies were found. Those in languages other than English, Spanish and French or without access to the full article were not taken into account. Those with relevance (published in the past 11 years, relation between labeling and consumption, systemic reviews, peer review) were selected based on the reading of the abstract by all the authors. Sixteen studies were included (of which four are systematic reviews) together with four meta-analyses, two of which were conducted on Mexican population (Table 1).
Studies
A study was conducted in Europe with 11,781 subjects from France, Germany, Poland, Sweden, Hungary, and the United Kingdom in supermarkets, in which buyers’ behavior was observed. It reported that a third of consumers in retail stores saw the label, but that only 16.8% used the information to determine their purchases (Storcksdieck & Wills, 2012). In some countries such as the United Kingdom, caloric content was color-coded with red, yellow, and green labels, regardless of the percentages of fat, carbohydrates, and proteins. Only 15% of people were found to read product labels (Sacks, Veerman, Moodie, & Swinburn, 2011).
Other department stores, however, reported no change in food purchases after labeling (Jeffery, Pirie, Rosenthal, Gerber, & Murray, 1982).
A study conducted with a control group in Minnesota with 400 consumers and eight supermarkets over 10 months reported that consumers improve their knowledge of food in terms of its content. However, no change in consumption preferences was recorded after foods had been labeled with their nutritional content, suggesting that knowledge of foods does not alter consumption preferences (Jeffery et al., 1982).
A study in Germany and Belgium showed that labeling had no impact on food consumption (Möser, Hoefkens, Van Camp, & Verbeke, 2009).
A specific meta-analysis of front-of-package labeling found arguments for and against it. It concluded that labels based on traffic light colors are most effective when they are accompanied by nutritional education for the population and that family food purchases are made on the basis of their affordability and the family’s economic capacity (Hunger et al., 2020).
Researchers in Australia found that monetary interventions (discount coupons for fruits and vegetables) in conjunction with improved food availability obtained better results than those based on nutrition labeling (Liberato, Bailie, & Brimblecombe, 2014). In the United Kingdom, a meta-analysis including 20,000 consumers and 800 stores concluded that the benefit of monetary interventions is greater than that of other interventions (Hartmann-Boyce et al., 2018).
Another systematic review of studies in the past 20 years of different interventions reports that the combination of the availability of fresh food and low cost, promotion, and information jointly determine consumer preference (Mah, Luongo, Hasdell, Taylor, & Lo, 2019).
Another study showed that labeling achieves effective results when it is accompanied by taxes added to products regarded as being less healthy (Acton, Jones, Kirkpatrick, Roberto, & Hammond, 2019).
Taillie, Ng, and Popkin (2016) provide a stimulating description of the role of supermarkets in nutrition and health and food availability. They note that new supermarkets, also called supercenters, selling products other than nutritional ones, offer more processed foods and fewer fresh foods. The presence of this type of stores has increased significantly, especially in rural and low-income areas, making large supermarket chains a key element in population nutrition.
Mexico and the United States
One study assessed the understanding and use of nutrition labeling systems by adult consumers in the United States and Mexico. Consumers in the US (White n = 2,959; Latino n = 667) and Mexico (n = 3533) were shown the five food labeling systems:
The Nutrition Facts Table (NFT).
The Guideline Daily Amounts (GDA), showing nutrient levels.
The Multiple Traffic-Light (MTL), which color-codes each GDA nutrient (green = healthy; yellow = moderately unhealthy; red = unhealthy).
The Health Star Rating System (HSR), which classifies foods in a single dimension of healthiness.
Warning label (WL) with a stop sign for nutrients present at unhealthy levels.
Participants reported a higher degree of understanding of WL front-of-package labeling (OR = 4.8; 95% CI [4.4, 5.3]) and a lower understanding of HSR (OR = .34; 95% CI [.31, .37]) and MTL labeling (OR = .56; 95% CI [.52, .61]), with similar patterns of understanding in all ethnic groups. The authors concluded that a brief summary of front-ofpackage labeling may be more effective in both the United States and Mexico in guiding consumers toward informed food choices (Nieto et al., 2019).
Another study explores the subjective understanding of labels used internationally among low- and middle-income Mexican consumers. The following front-of-package labeling systems were evaluated: NFT, GDA, MTL, WL, and HSR. Most subjects were aware of the GDA, but rarely used it because they found interpreting the information too complicated. Red warning labels were more accepted than black ones (Vargas-Meza, Jáuregui, Pacheco-Miranda, Contreras-Manzano, & Barquera, 2019). It is worth mentioning that both studies were published by the same people responsible for the front-of-package labeling program in Mexico, so there may have been a conflict of interest in both publications (Nieto et al., 2019; Vargas-Meza et al., 2019).
Patients with eating disorders (ED)
Regarding patients with ED, a study conducted in 2017 in Minnesota administered the EDE questionnaire to 716 female patients with an average age of 21 (Fairburn & Beglin, 1994). They were randomly assigned menus, some of which listed the calories contained in each food while others which did not. Patients included thirty people diagnosed with anorexia and bulimia and some others with binge eating. The group of patients with ED who were given menus in which calories were labeled selected foods with an average of 263 calories less than those in the same group who were given menus in which calories were not labeled. No significant differences were found in patients without eating disorders (Haynos & Roberto, 2017).
Some reports have found that when families unable to purchase other types of food products encounter these labels, they experience confusion and frustration (Draper et al., 2013).
A study conducted in the United States showed that overweight people choose their food based on taste or personal preferences rather than the labeling (Visschers, Hess, & Siegrist, 2010). However, people who consume food based on the number of calories they contain select their food based on the labeling. This group includes patients with eating behavior disorders, in whom labeling constitutes a significant barrier to their recovery process. Having access to this type of information in such an obvious, overt, way increases their anxiety levels (van Herpen & van Trijp, 2011).
One fact worth highlighting is that when labels with caloric content were added in fast food restaurants serving affordable food for the whole population, these restaurants reported that at no time did the sale of foods labeled as high in fat or high in sodium decreased. However, when these labels were added in cafeterias frequented by people from a higher socioeconomic bracket, they did modify food choices (Visschers et al., 2010).
Discussion and conclusion
Food labeling is one of the least successful regulations for curbing obesity since it fails to alter patterns of consumption in either people with low economic resources or most adolescents.
Although ENSANUT reports in Mexico use the Body Mass Index (BMI) as a diagnostic measure, we know this is not an effective means of measuring obesity.
The BMI is an index created in 1800 by an academic (not a medical doctor) whose object of study was to find “normal” averages, basing his study on French and Scottish men (Hughes, 2013). The BMI was not created to measure percentages of fat and health, or individuals, but populations. This index does not reflect the distribution of body fat and neither distinguishes between muscle mass or fat, or ethnicity. It may underestimate body fat in people who have lost muscle mass (sarcopenic obesity), and fails to adjust for physical activity or lifestyle, genetics, bone density, and other individual factors (Tomiyama, Hunger, Nguyen-Cuu, & Wells, 2016). It is less reliable in specific populations, for example, the elderly, people with physical disabilities, those under 18, people with severe obesity, during pregnancy, and in patients with ascites or severe edema (Bener et al., 2013).
Recently published Canadian obesity guidelines recommend a comprehensive evaluation that includes at least waist circumference and ideally a comprehensive evaluation of metabolic risk factors through the Edmonton Obesity Staging System (Sharma & Kushner, 2009; Jenkins et al., 2013; Hastie et al., 2009). It should be noted that life expectancy is not reduced by having a higher BMI. A recent study describes how women with a BMI of 27 have a longer life expectancy than those with lower indices, which has been called the “obesity paradox” (Islam & Hossain, 2017; Flegal, Kit, Orpana, & Graubard, 2013; The Lancet Psychiatry, 2020).
Survival of more than five years has also been reported in subjects undergoing percutaneous coronary intervention (PCI) in “obese” compared to “nonobese” subjects based on BMI (The Lancet Psychiatry, 2020).
Positive aspects of labeling include information to support the fact that the Mexican population living in various cultural and geographical contexts (in Mexico and the USA) has a comparable understanding of the information in the labels (Nieto et al., 2019).
Moreover, given that labels with numbers, percentages, or proportions are more difficult to understand for the average consumer, the straightforward design of labeling in Mexico can be considered understandable (Draper et al., 2013).
Literature reviews on the subject agree that despite the enormous number of publications (over 5,000), only a small number meet the requirements for inclusion in systematic reviews (Liberato et al., 2014; Mah et al., 2019). Furthermore, the heterogeneity of the interventions limits the number of studies that can be directly compared. It is worth mentioning that, although there are studies on labeling in Latin American countries, most available evidence has been produced in countries with high purchasing power (Hughes, 2013).
Although labeling can improve the education of the recipient population, this does not necessarily translate into a change in purchasing decisions even if the message is guaranteed to have been understood by the consumer (Roberto et al., 2012).
Experiences of other countries can be used as an example of interventions applicable to the Mexican context. It should be noted, however, that Mexico is a diverse country in economic, social, and educational terms. Moreover, there are differences in labeling preferences by gender, in that women prefer labels that provide information on the recommended percentages, whereas men prefer simpler labels, such as the food traffic light system (Möser et al., 2009; Hughes, 2013).
One aspect worth noting is that many studies that measure the effects of different types of labeling have been conducted in experimental settings (Acton et al., 2019), which is also true for Mexico. A study in Mexico was conducted in a low- to middle-income population in an urban environment, on the subjective understanding of labels and their acceptability. It was undertaken in an experimental environment (Gesell chambers), and it is unclear how the socioeconomic level was operationalized. Although it was reported that subjects were recruited in geographic spaces associated with this economic status, other sociodemographic factors are not reported, such as monthly income, or whether the person was economically dependent (Vargas-Meza et al., 2019).
At the same time, there is evidence that labeling can work in simulated or experimental environments, but not necessarily in the real world (Hughes, 2013). Other factors, such as logos and packaging design (Visschers et al., 2010), also influence consumer decisions.
Labeling is a strategy that is uniformly applied to the population, without considering the multiple factors that influence what kind of food to buy, such as purchasing power, age, gender, ethnicity, and the time available to make shop (Hughes, 2013). Consumer intentions also play a role. For example, the information included in the labeling may be assessed differently if the food is purchased for oneself or someone else, for children or adolescents, or if a health condition in the end consumer is considered from the very beginning (Visschers et al., 2010).
One of the least considered groups in public policy design is people who suffer from or have risk factors for eating behavior disorders. We found only one publication which considered this vulnerable group. It reported that, when exposed to labeling in an experimental setting, women diagnosed with anorexia nervosa accentuated restrictive food selection, while those diagnosed with bulimia nervosa increased the caloric content of their food choices (Haynos & Roberto, 2017).
The aim of improving the quality of Mexicans’ health during the pandemic is valid. However, during economic crises, labeling processed foods may create greater inequity in people who can only access certain foods, which in turn exacerbates obesity and leads to a lower quality of life. Labeling certain types of foods considered obesogenic fails by framing obesity as a problem exclusively linked to food intake without considering the genetic, metabolic, social, and psychological factors that contribute to obesity and eating behavior disorders (Hunger, Tomiyama, Nguyen-Cuu, Wells, 2016).
If health is the goal, reducing “obesity” is not the answer, nor is it sustainable at the population or individual level (Durso & Latner, 2008). Food labeling in the studies undertaken also failed to reduce the consumption of processed products. When laws proposed by governments are enacted using stigmatizing language, this may lead to the internalization of the bias surrounding weight, in which the individual approves negative stereotypes, beliefs and feelings about their status (Miller & Lumeng, 2018).
Policies that promote health can focus on improving the nutritional status of the population and providing opportunities for the entire population to engage in appropriate physical activity, as well as enhancing psychosocial factors such as psychological support, adequate rest, and stress reduction. Acting like this prevents shame for people who live in a larger body, thereby ensuring better engagement in sustainable behaviors that improve health and benefit all people across the entire BMI spectrum. These policies are particularly important for populations with marginalized groups. Low income is the leading cause of food insecurity in Mexico.
Regarding aggregate taxes in Mexico, imposing tax on sugary drinks and foods with high caloric density has focused on the fiscal purposes of taxation. Most of the population that consumes these foods is insensitive to these price changes, as a result of which the decrease in consumption is insignificant. Likewise, it is known that its extra-fiscal potential has been wasted, in other words, no specific mechanisms have been designed to monitor the destination of the funds obtained. No clear actions have been promoted to transform these resources into public goods and services that would really encourage people to adopt different habits, motivate them to consume other types of food, or create environments and ecosystems resulting in healthier practices.
Front-of-package labeling is considered a major social and political measure in the attempt to reduce obesity levels. However, there is insufficient scientific evidence to suggest that this type of labeling reduces consumption of processed foods in patients with obesity. Price, taste, and availability are much more important to most consumers than the information in the label. However, in people with a tendency to choose foods according to their caloric content, particularly those with a genetic or metabolic propensity to develop an eating disorder, this type of labeling can trigger the latter.
The problem of obesity associated with morbidities goes beyond having information on the food consumed. It is a deeper problem that encompasses financial aspects and access to fresh food. Politically speaking, this is complicated and labeling food is the simplest (and cheapest) attempt to make a much more complex problem disappear.
The most successful measures for reducing both obesity and eating disorders are those that do not classify food as “good” or “bad” and instead promote well-being and health, breastfeeding, family settings that encourage physical activities, varied menus, and the acceptance of the concept of health for all body types.